It would be remiss of me not to start my blog today without recognising the recent news of another round of Junior Doctor industrial action, from 24 to 28 February. This comes on top of a couple of incredibly challenging weeks for our emergency services and so we will continue to work together and plan for this latest round as always, with a key focus on maintaining patient safety and minimising disruption to routine care as far as we can.
But, this month, I don’t want to focus on emergency care, but would like to showcase a few other areas – that of our evidence and evaluation team, some of the ongoing work to improve our community and crisis mental health services and some key updates around primary care across Norfolk and Waveney.
Evidence and Evaluation
Across the NHS we see an awful lot of focus on the new – we like pilots, projects and change, and aren’t always very good at measuring the true impact of these changes, adopting them widely if they work, or dropping or changing them if they don’t work.
So our new NHS Norfolk and Waveney Evidence and Evaluation (EE) Hub aims to change this! The hub itself was initially a two-year project, funded by partners across our health and care system, with the specific aim of evaluating some of our big new projects. Things have moved on significantly since then. The team is now a substantive part of our ICB, and its developing programme of work now covers a diverse range of projects across the system.
The team are an amazing resource – not only can they undertake large evaluations of large projects, but they can also advise teams on how to evaluate their own work, how to implement evidence, and how to monitor their effectiveness.
They also undertake evidence reviews – to help people know what already works and what we actually just need to get on with and implement. A good example to explain this is statins.
These have already been proven to work. We already know who would benefit from them, and we know that if those people take them, we will prevent heart disease and strokes. So, there is no point undertaking an evaluation to prove this again locally, to count how many events we have prevented and the hub would say no to that as an ask. But instead they could advise on the best way to implement this evidence and to monitor how well that implementation is going.
Conversely, if we wanted to set up a new service to help people remember to take their statins that sounds like a good idea, but it has never been proven to actually work. So, that would be something that should be evaluated to find out whether more people actually take them after that intervention and if that is a cost effective intervention.
Recent examples of the hub’s work include:
- Evaluation of the Cancer Care Navigator Service.
This service aims to deliver personalised care for people diagnosed with cancer, to signpost them to other services when needs arise, and to provide emotional support to cancer patients.
The hub has evaluated the introduction of the service at each of our three trusts, and also provided a system level evaluation identifying where it has definitely made a difference and where things could be better. The evidence and evaluation hub is now working with colleagues at the Acute Trusts in an advisory capacity and further evaluation of the service will be carried out by the Acute Trusts themselves.
- Evidence review of outcomes of Electronic Patient Record (EPR) implementation in acute settings.
The hub produced an evidence briefing to synthesise current evidence in an accessible format for decision makers. They produced a briefing to summarise the outcomes of EPR implementation in other systems which has fed into the full business case for the new EPR system.
- Evaluation of virtual ward implementation across Norfolk and Waveney.
The evidence and evaluation hub is currently undertaking an evaluation of virtual ward services across the system. This includes an evaluation of the implementation and outcomes of our community-led “step up” virtual ward, and an assessment of the quantitative outcomes associated with the step-down virtual wards in the acute trusts across Norfolk and Waveney. Data collection will include interviews, surveys and provision of metric-based data during 2023 and 2024.
- Evaluation of the Research Engagement Network (REN), The team undertook an evaluation of this initiative to develop research engagement with diverse communities locally earlier this year which supported the project team in successfully applying for a second phase of funding. This second phase aims for people who experience disadvantage because of where they live or who they are, to understand and act on their own health, and share their views on what they want research to focus on and how research is designed and delivered in future – so that we focus on what matters to our communities. This has involved training staff and volunteers from 20 VCSE organisations to engage in conversations about research in health and care and share participation opportunities, recording, analysing, sharing and acting upon insights via the ICS Community Voices insight bank. The evaluation confirmed that this has supported the development of a VCSE-led network, which should enable sustainable infrastructure for increased diversity in research engagement in future.
Another evaluation the team has undertaken was that of Mental Health Crisis Alternatives which is a nice segue into mental health…
Mental Health
The team also undertook a mixed-methods evaluation of two mental health crisis support services operating in Norfolk and Waveney: The Mental Health Joint Response Car (MHJRC) and Evening Crisis Support Hubs. The evaluation outlines the impacts of these services which include provision of an appropriate place for support, reduction of pressure on emergency services and integration within the wider mental health support context.
I was lucky enough to spend an afternoon at the Rest Café in the beautiful Churchman house in Norwich last month. It is so good to see this building being used in a great example of where the VCSE and NHS meet. It is a regular cafe, but also staffed by MIND available for people with mental health needs to drop in for support. People can then be offered 6 weeks of one to one or various different groups for short term support. The same building then has a small sanctuary area for out of hours crisis support – NSFT and MIND working together – for people with acute mental health needs but who don’t have physical health needs as an alternative to an Emergency Department (ED).
People can be referred by ambulance, 111, police, community mental health teams or primary care. The evaluation found that around 350 people had used the evening service in a six-month period. The most common outcomes were de-escalation at the point of a mental health crisis and better preparing service users to recognise, manage, and prevent crises moving forwards. The service is holistic – notably in 198 instances the service was able to offer support to address the wider determinants of health, and they also found examples of service users who had previously attended an ED several times a week who have now been better supported through the hub when they are feeling lonely or vulnerable to receive care in a much more appropriate setting.
On Monday last week I also spent a few hours with the crisis team in Norwich. This is another collaboration – this one with EEAST and NSFT staff. As well as meeting various members of the team to understand how the service works, I also had a ‘blue lights’ ride with a senior emergency medical technician from EEAST and a mental health nurse from the crisis team undertaking a joint assessment for someone in their own home.
Almost all of their call outs come directly from the 999 stack, for people in crisis or from an ambulance crew on scene who have identified that the person actually had primarily mental health needs. During January, they had 110 referrals, of which 75% were people already known to NSFT. The vast majority 86% were assessed and treated on the spot and did not need to be conveyed anywhere, with follow up put in place for around 50%. This meant that they did not go on to be admitted via any other route within the next 48 hours either. As one of the mental health staff put when interviewed as part of the evaluation: “ED is the last place I want to send anybody in mental health crisis, it’s just not the right place for them.”
More recently, we have been focusing on the transformation of community mental health services. This has been a huge piece of work which aims to deliver:
- A place-based community mental health model aligned to PCNs including access to psychological therapies, improved physical health care, trauma informed care, medicines management, support for self-harm and substance misuse
- Modernisation of Community Mental Health Teams to shift to whole person, whole population health approaches
- A renewed focus on people living in their communities with long-term serious mental illness
- A new focus on people whose needs are deemed too severe for NHS Talking Therapies (TT) but not severe enough to meet secondary care “thresholds” including complex emotional needs.
This ambitious work has made huge strides, although there remains a massive gap to deliver on these ambitions as more people come forward who are struggling with poor mental health. Our team continues to work very closely with NSFT and wider partners to ensure we transform and improve mental health services for the people of Norfolk and Waveney, together.
To support these aims we have appointed 68 mental health staff working in general practice so far, using a combination of funding sources to appoint mental health practitioners and emergency response workers, working alongside primary care clinicians, as recognised by our shortlisting for a national award late last year.
We are also establishing a community interface service whereby those people whose needs are more complex can be discussed by a group of professionals in a local multi disciplinary team which can then direct that request for support to the most appropriate service – be that the Primary Care Network mental health team, the personality disorder service, sexual trauma support, Change Grow Live for drug and alcohol support, psychological therapies or specialist medical input.
Not all of these are in place yet, and there will be teething difficulties I know, but using the key principals below we know what we need to do, and how we can do it.
Please visit the webpage here for a lot more detail and direct any suggestions or queries through nwicb.mentalhealthteam@nhs.net.
Primary Care
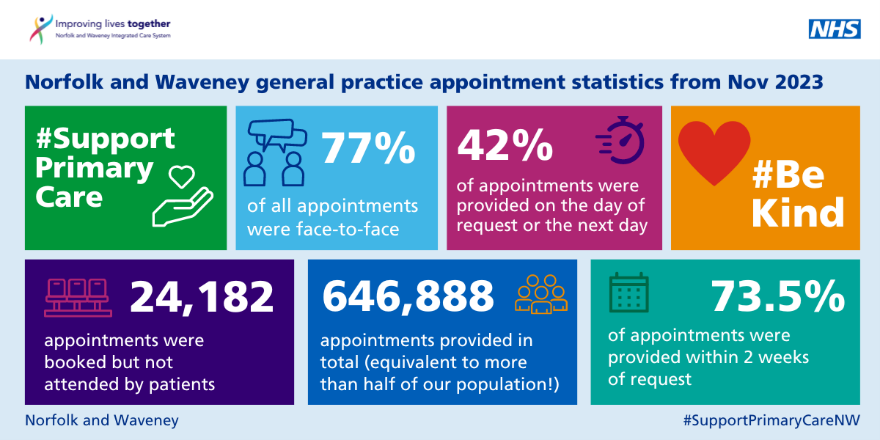
I’d also like to give a big shout out to our general practice colleagues, for yet another staggering month of activity. The graphic below includes the latest snapshot of recorded activity across general practice. More than 600,000 appointments took place in Norfolk and Waveney, 77% of which were face to face, and 230,000 of which were on the same day in just one month: November 2023.
As ever, the vast majority of the care we provide our patients is via primary care, and so it is more important than ever that we are aware of pressures in this area, and do all we can to support them. We now have a better way of tracking pressures in primary care. Thanks to the Norfolk and Waveney LMC, the General Practice Alert State Sitrep (GPAS) now comes out every week, which complements the national OPEL system for our other providers, and helps us better understand and support all partners in our ICS.
You may be aware that we are also engaging with our patients and communities across Norfolk and Waveney on our latest dental commissioning intentions and long term plans for the future. Please do share this with teams, colleagues, and patients and fill it in yourself! It’s vital we hear from as many people as possible.
Finally, I’d like to end my blog this month with a focus on medical leadership changes, both within the ICB and support for the wider health and care system.
Adverts for two of our trust Medical Director roles have just closed with interviews pending for the MD post at Norfolk and Suffolk NHS Foundation Trust; and the combined MD post across Norfolk Community Health and Care (NCH&C) and Cambridgeshire Community Services.
I’ve been lucky enough to help with the shortlisting for the NCH&C role and have met a few of the prospective candidates for the NSFT role too, so I’m delighted at the number and more importantly calibre of applicants for both.
Within the ICB, we are also about to see some flux. Dr Clare Hambling has been appointed national clinical director for diabetes and Dr Ge Yu has also been appointed medical director for primary care with East London Foundation Trust. So please join me in congratulating them both on these excellent appointments.
I’m also very sad to share that my Deputy Medical Director, Dr Andy Griffiths will also be retiring soon, though he is continuing to support our CCP leadership agenda and armed forces and veteran’s health until a new post holder is appointed. Andy will be hugely missed (especially by me!), but with these changes in mind, you will soon see a few new specialty advisor posts coming out soon.
And speaking of retirements – if any of you are planning to retire or have friends who have already, there is a national move to support more recently retired doctors to work flexibly. You can register your interest here – please do take look!
With thanks for everything you continue to do,
Frankie.
