Firstly, I would encourage you all to read the Chief Medical Officer’s annual report 2023: health in an ageing society by Chris Whitty. This is really useful in drawing attention to the issues facing the NHS across the whole country and particularly in Norfolk and Waveney. I think the report has two key messages for us. First, we must work to intervene earlier and aim to prevent ill health and frailty in later life, and second, that we need to work with our older residents to design and provide services best designed to support them.
I’m glad that the work to agree our Ageing Well strategy is going well. I’m hoping for this to be published in the next couple of months with our new board starting early in the New Year to oversee and coordinate the multiple strands of work to support this.
Secondly, please also have a look at the Three Hospitals, Three Weeks patient experiences at Norfolk hospitals report recently published by Healthwatch Norfolk. Their volunteers asked over 1,400 patients and visitors at our hospitals what they thought of their care and despite everything, the median response was a score of 5 out of 5, with a mean overall of 4.6 at JPUH and 4.5 at QEH and NNUH. So, while things aren’t perfect, we do have a huge amount to be proud of.
This month I will also focus on:
- Industrial Action
- Urgent and Emergency Care and winter
- Primary Care access recovery and interface
- Clinical and Care Professional Leadership
- Digital and Shared Care Record
Industrial Action
This is the first month in a while that we’ve not got any strikes in the diary and the unions and the government are back around the table. Talks do seem to be going well too, though clearly, we have another new Secretary of State for Health and Social Care – the fourth change since I’ve been in this role – with Victoria Atkins announced in the role on Monday. So, we will have to wait and see but I am feeling more optimistic than I have for some time on this.
It is also vital that we appreciate and reflect that despite these incredibly tough rounds of Industrial Action, we have done well. We are pulling together, we are keeping our system safe during the strikes, and we are continuing to press on – slowly, chipping away at the elective back log and reducing waiting times for our patients, so we must not lose heart.
Urgent and Emergency Care and winter
Urgent and emergency care is everyone’s business, and as a system more than 80% actually takes place in primary care every day. However, the highest risk and sickest patients will need the support of our emergency departments and often our ambulance service. The national target is for ambulance services to “offload” or hand over every patient to hospital emergency departments within 15 minutes. Unfortunately, this has been very difficult to achieve in our system and this means that in turn, people are sometimes having to wait far too long for an emergency ambulance to arrive in the community. Due to these and other pressures, our system has entered Tier 1 for Urgent and Emergency Care. Positively, that comes with a lot of visits, help and support from national agencies and partners and we have also made multiple improvements.
For example:
- We have been able to close the vast majority of our previous escalation and surge beds at our acute hospitals, e.g. having seven people in a six bedded bay.
- We have reduced the number of inpatients in our acute and community providers who no longer meet the criteria to reside (CTR) but cannot go home because they are waiting for reablement, social or other care out of hospital. This week that number was down to 230 non CTR patients in our acute trusts awaiting care on Pathway 1-3. Or if you count every single person who technically no longer meets the criteria for any reason, across all of our providers including community, then that number is 432 – where it peaked at 640 last year.
- A lot of this is down to improvements in social care and how our discharge hubs work. With Norfolk and Suffolk County Councils, we have brought multiple previous pilot services together, and expanded the funding and reach of them to launch the Norfolk and Waveney community support service led by Voluntary Norfolk, the British Red Cros and Age UK Norwich. This supports people recovering after a hospital stay and prevents readmissions.
- We also have a fantastic Unscheduled Care Coordination Hub (UCCH) which has been set up in the last few months. Again, this is an initiative that has grown out of successful pilots and is in line with national best practice. So, if someone calls 999 but on assessment they need help, but not that provided by an ambulance, they are reviewed through the hub. They work out what service would be best for that person, for example a two hour community response visit to help them up after a fall, or an out of hours GP appointment, or a Night Owl provided by the council etc. This means that the person gets the care they really need first time, and frees up ambulances to respond to others with more urgent health needs.
- We now have virtual wards set up at all three of our acute trusts to help people go home from hospital earlier, as well as the step-up virtual ward run by our community trust to prevent admissions in the first place. For primary care, if you have a patient you think would be suitable for this, please use the existing NEAT contact line and select option 2.
So – we’re making a lot of progress, but there’s much more we’d like to do, as however much we continue to expand other sources of help and encourage people to choose wisely, ambulances will always come and demand will always fluctuate.
There are three main areas of focus and our governance is built around achieving these three goals, as we know that this is our highest risk in terms of patient safety at the moment.
- Improve category 2 ambulance response times
- Reduce length of stay across all of our hospitals (including community and mental health)
- Deliver virtual wards
For this winter, we have pulled all of our ideas together to maximise the impact of all the resources that we have confirmed or indeed that might become available so we don’t waste any time on this.
This is our current list:
- Opening additional pathway 2 rehabilitation beds in our community
- Enhancing the UCCH and expanding support to residents of care homes
- Further strengthening of mental health crisis support
- Acute respiratory infection hubs as we ran last winter which reduced pressure on both Emergency Departments and Primary Care
- Additional transport to support more and earlier discharges from hospitals
- Cohorting space and staffing to help trusts continue to offload quickly even when faced with batches of ambulance arrivals and prevent long delays occurring at certain times
Primary care access recovery and interface
In May this year, NHS England published its Delivery plan for recovering access to primary care. It aims to tackle some of the pressures facing GPs and other services as we work to get back to normal after the pandemic.
The key ambitions are:
1. Empowering patients to manage their own health including using the NHS App, self-referral pathways and through more services offered from community pharmacy.
2. Implement Modern General Practice Access to tackle the 8am rush and avoid asking patients to ring back another day to book an appointment.
3. Build capacity through recruitment to additional roles with increased flexibility for the types of staff recruited and how they are deployed.
4. Cut bureaucracy and reduce the workload across the interface between primary and secondary care so practices have more time to meet the clinical needs of their patients.
The ambition is to reduce time spent by practice teams on administrative work and work generated by issues at the primary-secondary care interface to release more time to care for patients.
ICBs have been asked to establish local mechanisms which will allow both general practice and consultant-led teams from secondary care to raise issues, and to jointly prioritise and address them. ICBs have been asked to address these four key areas:
- Onward referrals: if a patient has been referred into secondary care and they need another referral for an immediate or a related need, the secondary care provider should make this for them, rather than sending them back to general practice which causes a further delay before being referred again.
- Complete care (fit notes and discharge letters): providers should ensure that on discharge or after an outpatient appointment, patients receive everything they need, rather than leaving patients to return prematurely to their practice, which often does not know what they need.
- Call and recall: for patients under their care, providers should establish their own call/recall systems for patients for follow-up tests or appointments. This means that patients will have a clear route to contact secondary care and will no longer have to ask their practice to follow up on their behalf, which can often be frustrating when practices also do not know how to get the information.
- Clear points of contact: ICBs should ensure providers establish single routes for general practice and secondary care teams to communicate rapidly, for example, single outpatient department email for GP practices or primary care liaison officers in secondary care. Currently practices cannot always get prompt answers to issues with requests, such as advice and guidance or referrals, which results in patients receiving delayed care.
There’s also a list of 10 “quick wins” taken from best practice around the country. We have delivered 5 of these already, with 5 more ongoing. Providers are also required to perform a gap analysis against the standard contract, then to develop an action plan to address any gaps. We will be sharing these at our public board at the end of this month. As an ICB we have a duty to oversee these and to hold providers to account against this contract but I think we should be proud of the progress we have made.
Some examples of good progress are:
- We have an interface group to work through knotty issues
- We have an agreed process to share issues in real time and we share the themes from these every month at our interface group and with all of our providers
- Fit notes remain a huge issue nationally, but the work we’ve done locally to address this has made a huge impact
- Clear points of contact have been established for both practices and providers to use to avoid waiting in general phone queues
- Shared Care Record now live for many though not all of our system just yet, saving huge amounts of time for those using it with 3,000 unique users in October, accessing 13,000 records (see more about this below).
Further reading on this by the Academy of Medical Royal Colleges can be found here and the Royal College of General Practitioners here.
Clinical and Care Professional Leadership
Our Integrated Care System is built upon the ethos of “Improving Lives Together,” and as we continue on this transformative journey, it is essential that we work with and listen to all of our clinical and care professionals.
The Clinical and Care Professional Leadership (CCPL) Faculty is a voluntary group of aspiring or established leaders from within Norfolk and Waveney who work within health, social care, private, independent, voluntary or education organisations who wish to be supported to develop system leadership skills. The faculty is free to join. Members can either self-nominate or be nominated by their employer. Once in the faculty members will receive regular updates and notification of role vacancies, stretch opportunities and training events.
We’ve just launched a new CCPL bi-monthly newsletter which we hope will become a valuable and valued resource for staying updated on our progress and upcoming initiatives. It’s a platform for us to share our achievements, address challenges, and foster a sense of community among our clinical and care professionals. It’s called The Integrator and you can read it here.
If you would like to join our CCPL Faculty or sign-up for the newsletter please fill in the on-line form. If you would like to take part in our CCPL follow-up survey, to help us develop and shape this vital area of work, please click here.
Digital
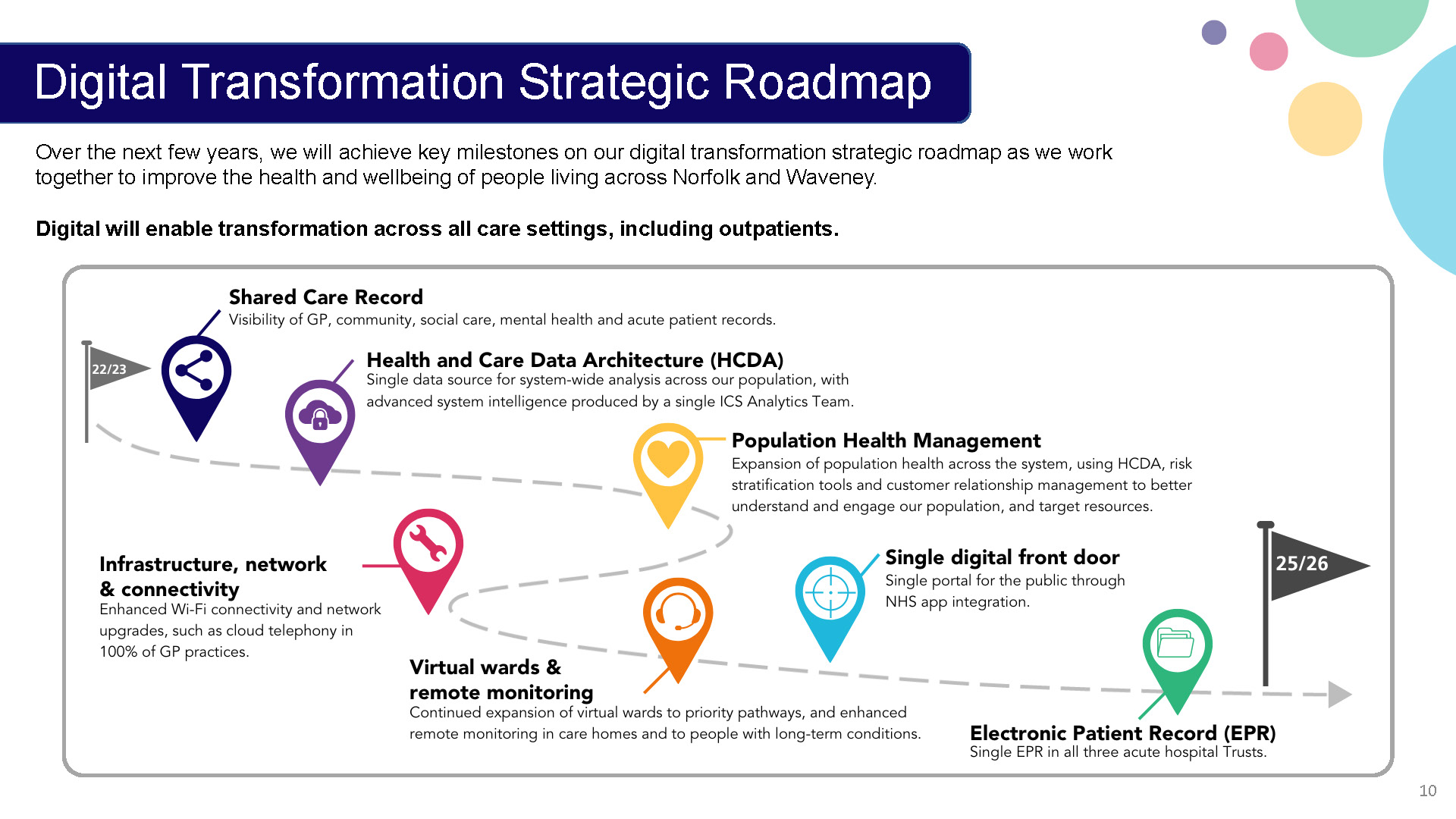
Our health and care system is evolving and to help improve people’s lives in Norfolk and Waveney, we are going to increasingly use digital tools and technology to transform care. Earlier this year, we published a digital transformation strategy and roadmap to help improve the lives of people and communities across Norfolk and Waveney. The strategy has three key ambitions it hopes to achieve:
- Improve people’s safety and quality of care
- Give staff more time to care for people
- Empower people to manage their health and wellbeing better
Key digital strategic transformation projects and milestones can be found below:
Shared Care Record
A key example of this is the Shared Care Record (ShCR) which has been rolled out in phases over the past year to organisations within the ICS. As of the end of November, all partner organisations will be able to access the ShCR and the system has received excellent feedback from users so far – around 3,000 users who securely accessed 13,000 records in October alone.
The ShCR gives providers instant access to the information we need to make informed decisions about the care we provide, reducing risks and saving hours previously spent trying to get through to other teams to find out the information needed now. This not only saves time for providers of health and care, but also reduces the need for people to have to tell their story over and over. It is streamlining our health and care processes, resulting in reduced waiting times and eliminating the need for redundant tests or procedures due to improved information sharing.
We currently have 33 Practices accessing the ShCR via SystmOne and are expecting the remaining practices to be accessing the ShCR by the end of the year. Staff within Norfolk Adult Social Care Services already use the system, saving them time when triaging referrals and making it quicker to support discharges from hospital. NSFT and the James Paget University Hospital are both already live, with their data feeding into the ShCR, and the Norfolk and Norwich University Hospital, The Queen Elizabeth Hospital and IC24 will all also be feeding into this very soon, once the final technical work to bring their data on board is in place.
Busy times, but I hope you’ll agree an awful lot to be proud of.
As always, thank you for everything you continue to do.
With best wishes,
Frankie
