After what feels like a really challenging summer, we are now planning and preparing for autumn and winter, which we know is always an incredibly busy time for health and care services. I know for many of you it will feel like there hasn’t been any let up over what are typically considered quieter months of the year for the NHS and I would like to thank everyone across the Norfolk and Waveney health and care system for your continued hard work and commitment.
I’d like to focus my blog this month on the following key updates:
- Industrial action, impact on UEC and elective activity
- UEC, including virtual ward
- Covid update and spotlight on NHS 111
- Update on General Practice activity
- NHS Norfolk and Waveney restructure
Industrial action, impact on UEC and elective activity
Junior doctors and consultants will undertake four days of joint industrial action across this month and next month. Of the 61,862 junior doctors entitled to vote in the ballot, 44,079 (71%) took part. Of those, 43,440 (98%) voted in favour of strike action. For consultants, 33,915 were entitled to vote, 24,106 took part (71%) and 20,741 (86%) voted in favour. For public health consultants the turnout was 38%, below the threshold for industrial action.
As a result, there will be four days of joint industrial action in September and October.
Strike days
- 19 September – consultants to provide Christmas Day level cover only, junior doctors to provide normal service
- 20 September – consultants and junior doctors to provide Christmas Day level cover only
- 21 and 22 September – full walk out of junior doctors, normal cover from consultants (though obviously not a normal service)
- 2/3/4 October – Junior doctors and consultants to provide Christmas Day level cover.
In previous periods of industrial action we have seen huge numbers of elective procedures, operations and appointments cancelled, primarily to divert consultant staff to support emergency care to backfill the junior doctors, but also due to the lack of supporting junior doctors in some elective areas. Generally, we have been able to reduce this number each time, but this time as the action is combined this is likely to be worse.
We have done all we can to minimise emergency demand during the strikes, and this combined with the availability of more senior decision makers, plus more space and flow in our trusts has meant that emergency care has been well maintained overall during previous strikes.
But, after the strikes, each time, it feels like we’ve then seen a really long tail afterwards – with poor discharge profiles, higher demand and more admissions for a few days, exacerbated by having very tired staff and some needing compensatory rest.
This time is different – the action is combined and as it is followed so soon after by a second round, we are treating the period as a single sustained incident and unfortunately this means we need to reduce our elective workload before, during, in between and after the action to maintain safety.
We don’t want to do this, but we don’t think we have any choice.
We are very sorry to the patients who are affected and their families and we’re also very sorry to primary care colleagues who are likely to receive more queries than usual from patients who are affected by this latest round of industrial action.
We continue to urge anyone to come forward to receive medical attention if they have a true emergency as normal, and to still attend routine appointments unless they have been specifically told not to come.
Thank you to all the staff involved, to clinical staff who will be working differently, as well as the massive workload on operational and administrative staff – helping to create new emergency rotas, plus reorganising elective schedules on a minute by minute basis, including speaking to patients, some of whom have had their appointments cancelled three times now.
UEC update, including virtual ward
All trusts are currently at a minimum of OPEL 3, some on full capacity protocol so they are still feeling very pressured with over 97% occupancy and escalation beds open. Community providers are also reporting high occupancy across inpatient units, and demand is having an impact on patients who the community trusts are providing ongoing care for at home, with an increasing number of unallocated visits which can spill into GP or hospital attendances if we aren’t able to provide that support in a timely fashion.
Non criteria to reside numbers are slowly tracking down towards 500. There are lots of factors behind this, but one major one is the fundamental mismatch between our demand for care for older people following their acute illness, and we have an older and more comorbid population than other systems, and our capacity in terms of community reablement beds and long term placements.
This gap is at least 125 for reablement pathway 2 beds and possibly more for pathway 3 beds, for patients being transferred to long-term care such as a residential care home or nursing home. But there is some good news with the opening of 48 new reablement beds at the Norfolk Community Health and Care NHS Trust (NCH&C) site in Norwich. We are also doing all we can to find additional capacity just as we did last year (when we opened around 200 extra beds), but we want to move away from short term to permanent.
The virtual ward expansion is also key to this currently.
- NNUH is currently at 60 beds, aiming for 93
- JPUH is currently at 40 beds, aiming for 48
- QEH is about to launch but aiming for 15 beds then 30 within the next couple of months as the integrated service with NCH&C comes on board.
NCH&C step-up beds go live on Monday 18 September, starting small and central to test the model and their workforce capacity assumptions then to inform the much wider roll out. West is next, all places should be live by December and these will be embedded with the home ward and rest of their UEC offer (so the same integrated team might also be doing a home visit on another person in the same home / a neighbour). Recruitment has gone really well. NNUH and JPUH are fully established, with NCH&C and QEH also doing well though not quite full yet.
Covid update and spotlight on NHS 111
Numbers are on the rise again with the current variant infecting people who’ve never had Covid-19 before, and with a slightly different clinical presentation: more headache, cold and flu or even hayfever like presentations. We also have some closed wards and bays in our acute trusts, and some care homes closed to new admissions because of outbreaks.
We have changed the way in which Covid medicines delivery units (CMDU) are organised. Since August, if a patient has a positive test and they are clinically extremely vulnerable they are told to call NHS 111. IC24 has a specially trained team to clinically assess these patients and if eligible they can issue a prescription electronically to one of 25 community pharmacies for oral treatment. This is available 7 days a week, 9am – 5pm. If patients call outside that time, they will be assessed in the usual way but will also be put into the clinical assessment service (CAS) queue so that a special Covid medicines delivery unit doctor will contact them in the morning.
This service supports high risk patients with symptoms in the last 5 days. Under 18s are under the care of a paediatric on call consultant, or if that’s not possible a GP. Treatments include antiviral medicines such as Paxlovid. Pharmacies also have a direct line (as do GPs) if they have a query about the patient or their treatment.
NHS England guidance is that this should be rolled into BAU for our integrated emergency care and primary care, so the plan currently is for this service to run this year only.
If patients are not eligible for oral medication and need intravenous (IV) treatment, they are directed to the Trusts. A long term solution is being sought in the hope that ultimately those people will receive their infusions via the virtual ward, though this is proving challenging to implement at the moment. If the patient has advanced renal or hepatic disease or is unable to swallow, then a one off IV infusion can be administered at the JPUH or QEH, with eligibility and assessment sitting with IC24.
Speaking of 111, I thought it might be useful to share some information about IC24, our 111 and GP out of hours provider.
Latest figures show that 28,700 calls were received in a month with 71% answered within 60 seconds. We do a lot to remind the public to call 111 first for urgent advice. IC24 has a trained team of health advisors who also work with CAS clinicians – typically these will be GPs, advanced clinical practitioners, or advanced nurse practitioners to provide more senior clinical input. They typically give advice, but can also make timed Emergency Department referrals, or book patients into see the GP out of hours service or home visits.
They also do a lot of work to validate calls – so if the advisor has recommended an ambulance is dispatched or the person to go to an Emergency Department, they will contact them to validate this. Similarly, they will proactively contact patients who are awaiting ambulances who have called 999 with their more senior clinicians determining if there is any other way to support those patients instead.
They also work as part of the urgent care coordination hub. For example, they will work with EEAST paramedics and CAS clinicians to review the inbound stack, requesting ambulances and seeing if there are any alternatives. They also support crews on the scene and are looking to support point of care testing (POCT) too. They can access SystmOne and Shared Care Record and use Feebris, the same monitoring technology we have in place for all of our virtual wards.
Update on General Practice activity
The Primary Care Access Recovery Plan was published in May and teams in the ICB have been working with local GP practices and community pharmacies to build up the foundations required to meet the aims of the national delivery plan.
This plan is nationally led and will build on work already happening locally in Norfolk and Waveney to improve patient access to services, but we know that it will take time to safely make all the changes outlined in the national plan. We’ve pulled together a news briefing to provide a little more detail for our patients about the recovery plan, what we’ve been doing to prepare for it already, and what it means for Norfolk and Waveney. Please take a look at the news item here.
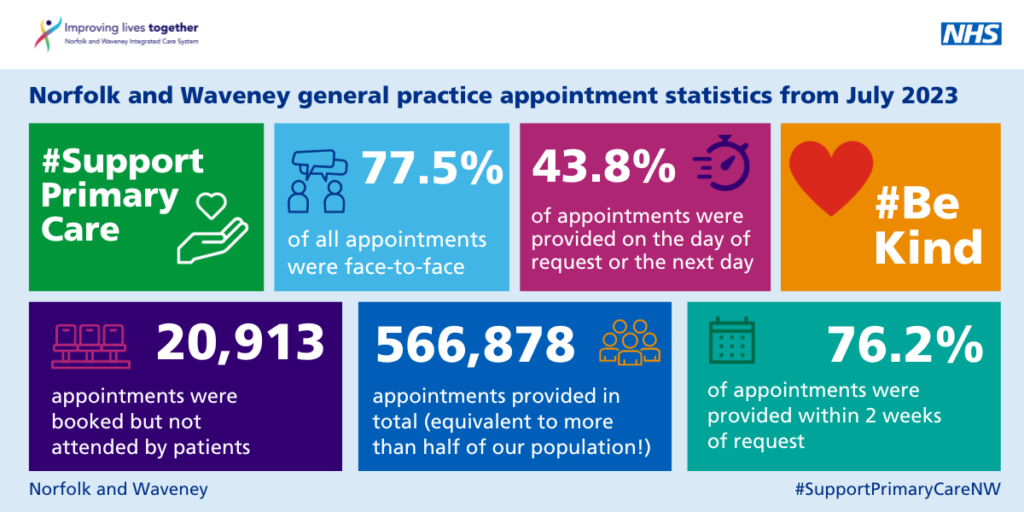
While all this hard work is going on, our GP practices are continuing to deliver exceptionally high levels of care for our patients. Here’s a look at the activity from July:
· 566,878 total appointments across general practice; although slightly down from the number of appointments in June it is still equivalent to more than one appointment for every 2 members of our population this month.
· We have slightly lower same day appointments than nationally (38.3% locally compared to 43.6% nationally), but that is almost certainly because we have a much higher proportion which are face to face compared to the national average (77.5% compared to 68.3%)
· 46.6% of appointments were delivered by a GP, and 51.2% by other practice staff. This mirrors the percentage nationally and is a fantastic reflection of both the exceptional levels of activity our GPs are delivering, and the increasing role of the wider general practice team in delivering timely and quality care for our patients.
· The handy little visual below provides a summary of activity across general practice in Norfolk and Waveney:
Progress with the NHS Norfolk and Waveney ICB restructure
The consultation period formally closed on 8 September and we are now taking stock of over 600 pieces of feedback both from staff potentially affected but also from multiple other stakeholders. This feedback will now inform changes to the proposed new structures and the final structure will be shared with staff on 28 September. There will also be a voluntary redundancy round open from the 25 September for three weeks with the final new structures hoped to be in place from April 2024.
Thank you for your patience with our teams in this period of uncertainty, and thanks to any and all who gave us feedback to try to improve our structures. It has been a very challenging situation, trying to essentially cut back £5.9 million of staff costs, is not one any of us wanted to be in, but we’ve tried to design our new structures to support the core duties of integrated care systems:
- to improve outcomes in population health and healthcare
- tackle inequalities in outcomes, experience and access
- enhance productivity and value for money
- help the NHS support broader social and economic development and our 5 year Joint Forward Plan priorities
There’s two other final items I would like to mention this month.
Women’s health hubs
Some funding has been made available nationally to support these. We are using a Population Health Management approach to define geographical areas of greatest need as well as Public Health data to identify highest clinical needs. We are planning a stakeholder engagement event during the first week of October, further details TBC.
Leadership changes
NCH&C and Cambridgeshire Community Services NHS Trust (CCS) have announced that Matthew Winn will be serving as Chief Executive across both organisations from 1 November 2023 for the next twelve months. Matthew has been Chief Executive at CCS since 2007 and has been the national director of community health in NHS England from 2019 to 2023.
Nick Hulme, Chief Executive of East Suffolk and North Essex NHS Foundation Trust (ESNEFT) has been appointed as the interim Chief Executive at the Norfolk and Norwich University Hospitals NHS Foundation Trust (NNUH). Nick has now started at NNUH and his appointment is until February 2024 while NNUH seeks a permanent CEO. He will remain Chief Executive of ESNEFT during this time.
Congratulations to Prof Erika Denton on her exciting six month secondment from NNUH to the National Medical Director team as Interim National Director for Transformation at NHS England. Erika will continue to support her team until an Interim Medical Director is appointed at the end of September. She will carry on with her clinical work at NNUH as well as some areas of her existing portfolio throughout her secondment.
With best wishes and thanks for everything you continue to do.
Frankie
