I’m now just over two months into my new role as Medical Director for NHS Norfolk and Waveney, and it’s been great to continue to get out and about and to meet lots of new people and organisations, particularly across primary care.
There’s so much in the press about primary care that I thought I’d start with some stats here for this month.
Despite enormous pressures, we are delivering more appointments in primary care than ever before – around 25,000 a day in July, with 72% being face-to-face (against a national average of 65%). More than 80% of our primary care appointments are already delivered within 2 weeks, and more than 40% take place on the same day too. In fact, 80% of our emergency health contacts currently take place in primary care!
And our patients report overall satisfaction or a ‘good experience’ of 76% (against an average of 72% in the recent national GP patient survey). 5 of our teams are also up for awards in the General Practice Award this year, so massive thanks and well done to all of our staff currently working in primary care. You’re doing an amazing job.
I also want to update you on the progress of the items I shared with you in my August blog.
Since last time, we have a new secretary of state, who has announced her focus on ABCD: ambulances, backlog, care and doctors and dentist.
The four top priorities for NHS Norfolk and Waveney are unchanged from last month, and the first two of these are very much aligned to the SoS’s priorities already:
- Urgent and emergency care (UEC) pressures and of course this isn’t just about ambulances but is also about having sufficient social care to support hospital discharge, as well as access to enough doctors in primary care
- Elective recovery is directly about addressing the backlog
And the last two priorities are more Norfolk and Waveney specific:
- Mental Health Transformation and
- Addressing our system financial deficit
Winter planning, Urgent and Emergency Care pressures and virtual ward
This neat little chart below shows a high-level summary of some of our progress across urgent and emergency care.
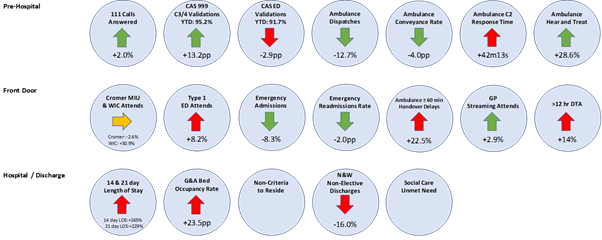
As a system, we are doing well on those prehospital workstreams: more people are using 111 and more of these calls are being answered; we are diverting more patients from 999 to 111 and our community response teams, 12.8% fewer people are being conveyed to hospitals, and 28.4% more people are given advice that means they don’t actually require an ambulance call out “hear and treat”. Our hospital front doors are also doing better – 8% fewer emergency admissions, 2% fewer readmissions, 2.9% more streaming despite an 8% increase in Emergency Department type 1 attendances.
But, where we have much more work to do is relating to patient flow. The number of people in hospital for 14 and 21-days has roughly doubled compared to a year ago, and the number of discharges has fallen. This means that bed occupancy is up across all of our system, community and mental health units as well as our acute hospitals, and far too many patients don’t meet the national criteria to reside. So this is where we are really focusing at present.
We have additional funding to help create extra capacity for winter; but with unanimous agreement that we don’t want more acute beds as we already have more people in our hospitals than need to be there. Instead, we are planning to use this largely to support discharge: to create the equivalent of an additional 250 beds in terms of community or social care support.
We’ve also been successful in our bid to ramp up our virtual ward from around 50 currently to 173 by April 2023 and to 370 by 2024. We have been busy recruiting additional clinical leads, and we are focusing on expanding the current service this winter, largely aiming at supporting people to be discharged from acute trusts earlier. But, longer term our vision is for a single team working as a hub, overseeing a much broader virtual ward for admission avoidance (step up) as well as reducing length of stay (step down) across our ICS. Virtual wards are incredibly popular with patients – after all, who wants to stay in a hospital if you could be supported to get better at home – but they also have fantastic outcomes with lower readmission rates, better quality metrics and lower mortality too for some pathways.
Next up mental health transformation
A couple of weeks ago saw the anniversary of the publication of the Jeesal Cawston park report into the deaths of three individuals in the care of a private hospital for people with learning disabilities in Norfolk. The hospital has since closed. Whilst the event led by the Norfolk Adult Safeguarding Board and partners recognised many improvements and work done following the report, there is clearly more to be done.
Norfolk and Suffolk NHS Foundation Trust also remains in special measures and last month saw the publication of a letter from their consultant staff committee expressing their concerns, and the Norfolk Health oversight and scrutiny committee (HOSC) has also focused on this area this month.
There is an enormous amount of improvement work going on within NSFT which we are supporting. This is focused on safety and addressing the condition notice and CQC must dos, as well as developing an open and learning culture across the trust, improving their governance, and finally looking at the demand versus capacity of the current services. The CQC have just spent two weeks visiting various inpatient and crisis units and I know that they have been impressed by the passion and commitment of the staff and service users that they have spoken to. No formal feedback yet and they are now looking forward to the formal well led inspection due in November.
Jossy Pike has also been appointed as Acting Director of Mental Health Transformation, for NHS Norfolk and Waveney. Jossy’s focus is on managing mental health system structural and governance transformation working closely with the existing mental health transformation programme.
The programme will look closely at demand and capacity. We want to be able to provide the highest quality specialist support to those who really need it, and to provide this as early as possible. But many people do not need such specialist services, the advice and guidance service from NSFT clinical pharmacists and new mental health practitioner roles based in GP surgeries as well as a broad education programme should help many more people get access to the support they do need as early as possible, and to prevent the need for escalation wherever we can.
We have doubled the number of mental health practitioners in our Primary Care Networks; we now have 37, as well as our enhanced recovery workers recruited through Mind to be first contact practitioners working with our primary care teams.
Locally, our IAPT (improving access to psychological therapies) service has also expanded, supported by Protect Now teams and we’re getting great feedback from the online apps Qwell and Kooth for adult and children and young people.
We also now have five drop in hubs, providing timely local mental health support: Norwich, Great Yarmouth, King’s Lynn, Thetford and Aylsham now all have a Steam or REST mental health wellbeing hubs. These are run in partnership with MIND and the Access Community Trust and people can drop in and access these directly, or be referred there by 111, the ambulance service and primary care. All hubs also have an Evening Sanctuary offer, accessible by emergency services or 111 Mental Health Option which provides crisis support to people as an alternative to going to the Emergency Department.
We also have a short stay recovery unit: Holly Tree House in Norwich. This amazing facility is run by MIND for us, where people with mental health distress can stay for up to five days respite, another amazing resource to try to avoid people reaching crisis point requiring a formal admission to hospital. This facility currently has four beds, but we are hoping to open two additional sites soon in East and West, with access to these led by the crisis recovery and home treatment teams.
I’m also really pleased to see that Mental health support teams are expanding in schools. Cambridgeshire Community Services NHS Trust will be providing this vital service and mental health practitioners are currently being recruited to increase this important support as we expand the service across our schools.
We’re also hoping to develop mental health support units at or close to our three acute hospitals. These will be staffed by specialist mental health practitioners from NSFT, who will provide specialist assessment and care for patients attending our Emergency Departments who require psychiatric input and to oversee discharge, diversion to a hub/sanctuary and or admission where necessary. We’d also like to expand the input of MIND into our Emergency Departments in due course to broaden and integrate the support available. We want to make it as easy as possible for people to get the help they need fast, so pulling together, sharing and simplifying all of these services is vital.
Clinical and Care Professional (CCP) Leadership
Thank you to everyone that has attended the various engagement events we’ve held so far relating to our Clinical are Care Professional Leadership framework. The formal launch workshop was facilitated by NHS England a few weeks ago. More than 90 people attended from all our sectors which resulted in a really valuable discussion. Three big take away points from that workshop and work so far are as follows:
- We are reviewing all of our structures and in time, we will ensure that we have a Clinical or Care Professional included in every decision-making body
- We will be recruiting to a new Clinical and Care professional Assembly to replace the previous CCTG and clinical executive. Think of it as a council of wise heads, reflective of all of our clinical and care workforce for ICS teams to sense check ideas with.
- We will be rolling out ongoing training and support to empower Clinical and Care Professionals in continuous improvement. You don’t need permission to try new things and to innovate, but we will support with Quality Improvement methodology, leadership training, and in evidence collection and evaluation. We are determined to harness your ideas, to try new things and learn from each other to improve things from the ground up.
Our series of masterclasses starts this week – click here to check the list of dates and topics and to access the links to join. All welcome!
As part of these masterclasses, these PowerPoint files provide additional information which highlight the importance of developing an effective ICS with a clinically and care professionally driven culture. They also show very clearly why you are critical to its success:
Interface issues between primary care and other providers
This month, I also wanted to provide an update on the Norfolk and Waveney primary, secondary and community care interface group.
We have agreed the principal that referrals from private providers should go direct to hospitals rather than back to primary care for an onward referral. We hope this will speed things up for patients, reduce risk and reduce workload for primary care once we’ve got the formal processes in place.
We have also agreed a new process for minor pathway changes, changes to referral forms and such like. All new changes should be made through a single point, the ICB Planned Care Team nwicb.plannedcareandcancerteam@nhs.net
They will assess the request, liaise with the Local Medical Committee and providers directly to make sure that there it has been planned correctly and there aren’t any unintended consequences to the change and if approved, they will take on the necessary communications, and changes on Knowledge Anglia etc. But, if it is not straight forward, or looks to be out of kilter with our contracts or other plans, then it will be diverted to the Interface group so that primary, secondary, community and mental health teams can collaborate to try to find the best solution together.
Where significant service changes are proposed, these will go through the existing governance routes and will be re-directed where necessary. I know this is very operational and process-focused, but I wanted to share what we discussed and agreed as little things like this can sometimes make day-to-day life much easier or more difficult when we get them wrong.
Finally, a couple of other bits and pieces to flag.
Please remember that nationally, all patients will be able to access their primary care records including all correspondence received after 1 November.
Also to remind you that we are gradually rolling out the medical examiner service with the aim that by April next year, we will be providing independent scrutiny of all community as well as hospital deaths.
So, as you can see, we are continuing to work at pace, together, to address some of our historic challenges. We need sustainable, long-term solutions to improve the health and care outcomes for our people and communities, and we can only do that together. We are also determined to make it as easy as possible for health and care professionals to have their say to improve our services, and to help make Norfolk and Waveney the best place to work in health and care.
Thank you again for your hard work, professionalism, and kindness, and please keep those ideas coming!
My next open medical staff meeting is on 11th October from 1pm – 1.30pm
With best wishes,
Dr Frankie Swords.
