Project outline
Implementation and embedding of a Maternal Medicines Centre (MMC) at the Norfolk and Norwich NHS Trust, within the East of England Maternal Medicines Network (MMN).
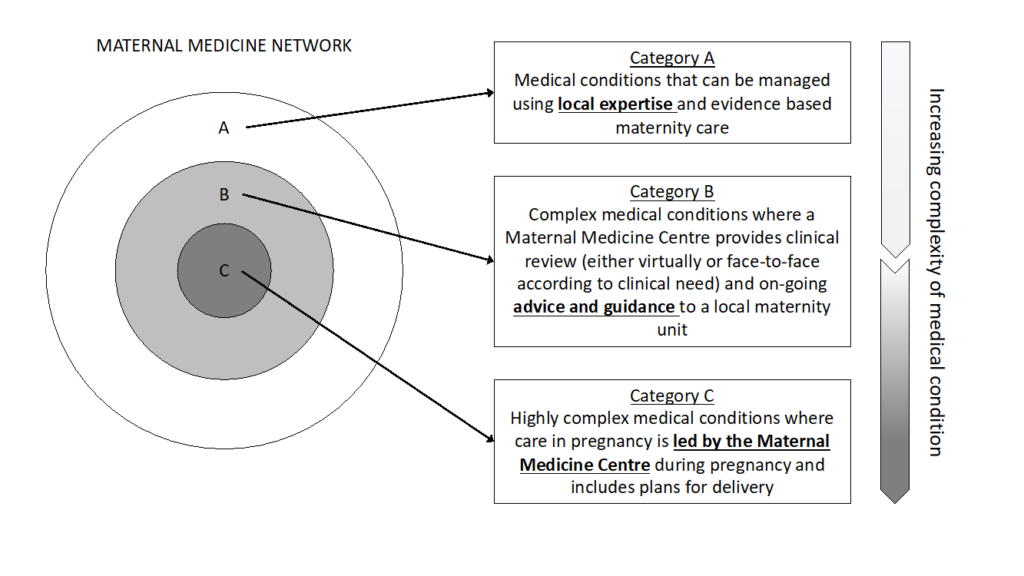
The MMN is responsible for ensuring that all women in the network’s footprint with significant medical problems will receive timely specialist care and advice before, during, and after pregnancy. All constituent providers within the network will be responsible for agreeing and upholding shared protocols on the management and referral of women with medical conditions, including reviewing guidelines and referral pathways.
This model of care will ensure that – where agreed appropriate – investigation and management is carried out by an experienced MDT that includes an appropriately trained obstetrician eg with sub-specialty training in maternal fetal medicine or equivalent; an obstetric physician or equivalent physician with appropriate training; and an appropriately trained midwife or team of midwives.
An MMC, hosted by Norfolk and Norwich University Hospital NHS Trust, will provide regional clinical leadership – on the identification, referral and management of women with medical conditions, including co-developing guidelines and referral pathways. In addition the MMC will ensure that appropriate education is in place across the network for all clinicians – ie midwives, obstetricians, GPs and emergency department (ED) staff – to improve local identification and referral of acute issues that have particular significance in women who are or have recently been pregnant. The MMN will need to work with other relevant networks including clinical networks for maternity services, perinatal mental health networks, neonatal operational delivery networks (ODNs) and fetal medicine services to ensure the health needs of mother and baby are met.
Why is this project needed?
Maternal medicine is the specialist care of pregnant women with either pre-existing medical disease or who have specific pregnancy related diseases that can affect any organ in the body. The incidence of maternal deaths from indirect causes is not falling in the UK at the same rate as direct deaths. 68% of women dying in the most recent MBRRACE-UK (2021) report had medical co-morbidities (excluding obesity) and in 41% of cases, assessment identified improvements to care which may have made a difference to the outcome. Maternal medical conditions are also significantly associated with neonatal morbidity and mortality.
The formation of a maternal medicine network, as recommended in Safer Maternity Care (DoH, 2017) aims to deliver co-ordinated and specialist care for women in the region with complex medical conditions.
The maternal medicine network is made up of Maternal medicine centre (hub) and Local maternity centres (spokes).
Supporting documents
Expected outcomes
Quality statement – aim of service
- To provide advice and planned care for women with pre-existing medical conditions, before, during and after pregnancy – ensuring equitable access, excellent experience and optimal outcomes for all communities served by the service.
- To provide advice and planned intrapartum and postpartum care for women with medical conditions that arise during pregnancy
- To provide local clinical leadership on the identification, referral and management of women with medical conditions, including reviewing training, clinical guidelines and referral pathways for all staff in contact with pregnant women across the footprint.
- To reduce inequities in pregnancy outcomes relating to medical complexity across all demographics
Table 1: NHS Outcomes Framework Domain:
| Domain 1 | Preventing people from dying prematurely | X |
| Domain 2 | Enhancing quality of life for people with long-term conditions | X |
| Domain 3 | Helping people to recover from episodes of ill-health or following injury | X |
| Domain 4 | Ensuring people have a positive experience of care | X |
| Domain 5 | Treating and caring for people in safe environment and protecting them from avoidable harm | X |
Project successes so far
The MMC has been successfully launched at NNUH in May 2022 with the Multidisciplinary team and governance in place. The LMNS has approved the funding proposal and a project manager has been appointed to support with reporting and service user engagement.
A task & Finish Group has been set up to continue to learn, improve and evaluate the new service.
