Project outline
Following on from the National Maternity Review in 2016 and the publication of the Better Births report, Maternity services in England have been tasked to achieve safer, more personalised care for women and families. Central to this is the implementation of Continuity of Carer. LMNSs should ensure that all providers remain on track to offer Midwifery Continuity of Carer as the default model of care and are prioritising rollout to those most likely to experience poorer outcomes. The building blocks for safe and sustainable transformation should be in place prior to roll out as set out in: Delivering Midwifery Continuity of Carer at full scale (LMNS deliverables 22/23).
Why is this project needed?
As a key deliverable of the Maternity Transformation Programme, maternity care provision through the Continuity of Carer model is linked to significant improvement in maternity outcomes, as well as improved satisfaction from women and birthing people, particularly for those who are most likely to experience poorer outcomes (NHS LTP, 2019).
Supporting Documents
Expected outcomes
MCoC to become the default model of care, resulting in improved maternity outcomes; reduction in preterm deliveries, stillbirth and neonatal death particularly for women of Black, Asian and Mixed ethnicity and from the most deprived neighbourhoods.
Project successes so far
Implementation of MCoC at the James Paget Hospital: approximately 83% of JPUH total pregnant population are being cared for under the MCoC model. This includes approximately 96% of all pregnant people from minority ethnic backgrounds and 88% from the most socially deprived areas. Locally sourced data has shown improvements in maternity outcomes, staff and women’s satisfaction with their maternity care:
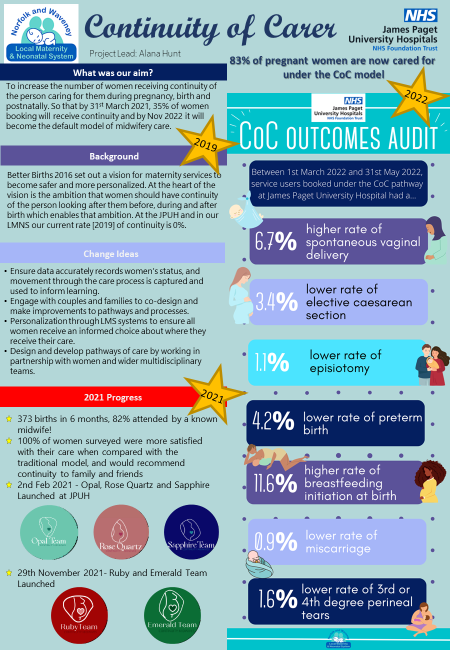
A co-designed survey hosted by Birth Voices East website from June-November 2021 received 72 responses from pregnant people who received MCoC care at JPUH. When rating their satisfaction with their care, all pregnant people reported 8/10 or above, with the majority (83%) scoring 10/10. 100% pregnant people felt supported with their birth choices and 96% felt they had opportunities to discuss their birth preferences
Plans have been submitted and preparations made to begin implementation of the MCoC model at the Queen Elizabeth Hospital and Norfolk and Norwich Hospital when all of the building blocks are in place.