April and May are always busy months, with Easter and bank holidays, but this year we’ve had an extra bank holiday and industrial action to contend with too. Everyone has played their part and gone above and beyond to ensure our patients receive safe care. Thank you to everyone working so hard across the Norfolk and Waveney health and care system.
Junior doctors industrial action took place last month and I was pleased to see how our system responded to this. It is important we understand and appreciate the reasons why junior doctors took part in the action, but also to the many thousands of staff who worked to ensure we could provide care to those who needed it the most.
Our eight immediate priorities remain I will focus on just a few of these this month in particular how they’ve been impacted by recent Industrial action, and then changing tack slightly – a look forward to the horizon with some updates on workforce and research.
Industrial action update
Junior Doctors industrial action took place between 11 and 15 April 2023. There were essentially no derogations during this action, meaning that care had to be provided very differently across our Acute Trusts in particular as Norfolk and Suffolk NHS Foundation Trust (NSFT) and Norfolk Community Health and Care (NCH&C) NHS Trust do not have large numbers of junior doctors.
Then, the Royal College of Nursing Industrial Action followed over the May Bank Holiday. This largely affected Norfolk and Norwich University Hospital NHS Foundation Trust, NCH&C and NSFT. Minimal derogations were made nationally although some were made during the industrial action for CCU and stroke services.
As a system we did well. Thank you to everyone who helped us to keep our service safe and flowing. I’m particularly pleased at how well we took the learning from previous industrial action and built that into our planning for these. We did a lot of additional communications and engagement work to warn the public what to expect, to choose wisely for emergency and urgent needs, and to increase awareness of why some appointments were affected. There was also a massive focus on discharge planning in advance which made a huge difference.
Please take a look on the dedicated section of the ICS website is available including the latest information, along with a dedicated frequently asked questions section. This provides the most up to date source of information for our system.
And please use our #WeCareTogether website as your single point of access for free health and well-being resources, free for all staff.
Elective recovery
Our target was to clear all the patients waiting 104 weeks by July last year and to maintain it, then to clear all those waiting 78 weeks (18 months) by the end of March 2023.
We had some specific challenges with specialist workforce in gynaecology with some patients breaching for that reason. But otherwise, we did incredibly well – missing the target by just 315 patients across our whole system despite large numbers of appointments which had to be rescheduled due to the industrial action in March.
Thank you to all who have worked so hard to achieve this, while striking the balance between maintaining elective care for people with very high clinical priority (such as those needing planned cancer treatments), as well as providing care for those people who have waited far longer than we would like for their routine planned treatments.
Our next major target is to clear all those waiting 65 weeks by the end of March 2024 and at the same time, push to keep improving our cancer performance, in particular the faster diagnostics 28-day standard.
We should all be very proud of what we have achieved here and of our combined efforts to keep on clearing the backlog and reducing our waiting lists. Thank you.
Urgent and emergency care
Despite all the recent industrial action, things are getting better here too. As a system, we stepped down from Critical Incident a couple of months ago and just before Easter, stepped down to OPEL 3. This is largely due to improving discharge as demand has not particularly let up, and we know that makes a key difference to flow through our Emergency Departments, acute and community hospitals. This means that patients are waiting much less time to get into or indeed out of Emergency Departments, which in turn means that ambulances are able to respond much more quickly, in line or close to national targets, for when emergency calls come in.
The number of positive COVID-19 in-patients in our hospitals continues to slowly fall, currently around 50, with one patient in hospital with flu and none with Norovirus (12 May 2023).
We are slowly and carefully closing our escalation and surge beds – this dipped to 120 pre bank holidays and is at 174 today, though we still have a long way to go. So, we need to continue a relentless focus on discharge, reablement and on internal processes to help more people leave hospital as soon as they are well enough to.
Primary care update
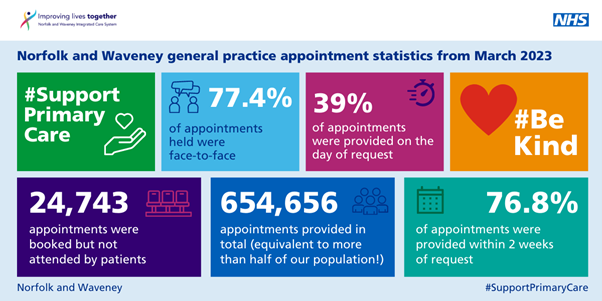
The latest data published shows that for March 2023, there is no let up in the massive demand and extraordinary scale of primary care provision in Norfolk and Waveney. This summary below shows a snapshot of our latest activity data. Around 80% of all of our emergency contacts continue to be provided in primary care!
Transforming care for older people and end of life care
Ian Hutchison, Chief Executive Officer of East Coast Community Healthcare has agreed to be our system Senior Responsible Officer for this important programme of work. Zena Aldridge has also joined us as our CCP special advisor for older people and dementia. Together, we are planning a workshop 23 May to design the Ageing Well programme. This is a really exciting opportunity, at which we will be bringing together representatives from the VCFSE sector, including older people themselves, district and local authorities, primary care and our NHS providers to really focus on what we would all want in an ideal world. Then we will be working back from there – to see what we need to start, to stop and to change to try to get there over the next three years, as well as leading major work to better publicise and coordinate some of the amazing services we already have.
Palliative care update
ICBs across the country now have a legal duty to provide and commission palliative care services to ensure people receive the care and support they need to live and to die well. This is the first time that this has been a legal requirement and there is lots of guidance and a national delivery plan for ICBs to improve access, quality and sustainability.
Palliative care provision across Norfolk and Waveney is currently patchy, with clear inequalities persisting. We are committed to radically improving and levelling up this care. Caroline Barry has been appointed our specialty advisor for palliative and end of life care and she will be chairing our programme board to lead on this, again working with patients and their carers, the VCFSE sector and primary care, acute and community providers.
Workforce
Clinical and Care Professional Lead Specialist Advisor update
I am delighted to share that we have successfully appointed to all the planned care, PHM, inequality, place leads, mental health, primary care lead and deputy Medical Director roles. There are a few more roles to be filled and interviews will take place over the coming weeks for children and young people, but I am really pleased with number, breadth and calibre of applicants.
I would like to specifically highlight that we have recruited to a number of important place lead posts, as follows:
- Dr David McConnell: Locality Lead – East
- Dr Ge Yu: Locality Lead – South
- Mrs Tracy Williams: Locality Lead – Norwich
- Dr Imran Ahmed: Locality Lead – West
- Dr James Gair: Locality Lead – North
In line with our priority to better support primary care, we have also appointed a Primary care CCP lead. Congratulations to Dr Jeanine Smirl for taking up this vital role. And we have just announced that Dr Andy Griffiths OBE will be joining us as the new Deputy Medical Director for NHS Norfolk and Waveney. Andy is due to start on 1 August 2023 and you can read more about his appointment here.
So as you can see, lots of vital work taking place to make sure our clinical and care workforce is both represented and supported at every level across our ICS.
As a reminder, please do take a look at the CCP landing page which carries our manifesto, rolling leadership programme and lots more details of how to get involved.
Our workforce – looking to the future
It’s incredibly early days, but I am excited to share that The University of East Anglia (UEA) is planning to open a Graduate Entry Medical school. The first intake is likely to be September 2025, but this could be wonderful for our system, specifically targeting local graduates to undertake a shorter course, building in HCA training from year one, with a real focus on inequalities, prevention and primary care based in one of three hubs across Norfolk and Waveney.
Similarly, although we’ve not been supported with a bid for a standalone school of dentistry, UEA are also pressing ahead with plans for a school of dental development and we are working closely with the University of Suffolk and exploring the possibility of a treatment and training centre in Lowestoft for people unable to access an NHS dentist.
Research and Our Future Health
You may have already heard directly about a large-scale, national research programme called Our Future Health. This research study is a collaboration between the public, private and third (charitable) sectors, established to develop new ways to prevent, detect and treat disease including cancer, dementia and heart disease. It also seeks to develop a strong industry base in Artificial Intelligence (AI), health and diagnostics as part of the governmental AI and Data Grand Challenge mission.
Our Future Health want to recruit five million adults from across the UK. Recruitment will likely start in Norfolk and Waveney in July 2023. Volunteers will be asked to complete a lifestyle questionnaire online and, at a face-to-face appointment, provide a blood sample and have some physical measurements taken. These appointments will take place at the Boots Pharmacy at Longwater, Norwich. Volunteers may be offered the results of their finger prick blood test, for example cholesterol measurements and their physical measurements, for example blood pressure. In future volunteers will be asked if they would like personal feedback from samples, DNA or other data.
As soon as more detail is available, we will be preparing and sharing more detailed briefings for general practices and Primary Care Networks about this research programme.
There’s lots of work to do, but by working together, we can all work towards ensuring that our patients, their families and carers have the support they need at the right time and right place.
As always, thank you for everything you continue to do.
With best wishes,
Frankie
