Can you believe we are in August already? The sheer volume of work and activity we continue to deal with is huge and I think this is one of the reasons why this year appears to be flying by so fast.
In this month’s blog, I want to focus on three core areas; Industrial action, and the impact this is having on urgent and emergency care and on elective activity; primary care, specifically general practice and the proposed staffing restructure for our Integrated Care Board.
Industrial action, impact on UEC and elective activity
Collectively, we have now dealt with five rounds of junior doctor industrial action, one round of consultant strike action, with the next round of junior doctors’ industrial action due to start at 7am on Friday 11 August running through to 7am on Tuesday 15 August 2023.
The next consultant strike will take place on 24 and 25 August 2023, with further dates just announced for consultants on 19 and 20 September 2023.
We are once again doing a lot of public facing communications activity to try to reduce demand, including our recently launched happy health holidays campaign, aimed at raising awareness with those who work and live in Norfolk and Waveney as well as those who visit on holiday at this time of the year. We see hundreds of thousands more people come to Norfolk and Waveney over the summer which is wonderful, but this does add pressure to our system, and many will not be aware of how to access health care support if they need it.
The campaign is set to last until the middle of September and will include adverts, both on and offline and communications direct with holiday companies, caravans and campsites who have agreed to share information when guests check in. The key objective here is to make sure that people use our services wisely, particularly those who are not familiar with our services so that people don’t simply go to our emergency departments by default if they develop an issue while they are visiting our beautiful county.
Thank you to all who are working differently during the strikes yet again. Huge numbers of our medical and other clinical staff are working extra shifts, in areas they don’t necessarily usually work in and undertaking roles that they don’t necessarily usually undertake as well. I am sorry that so many of us are tired and having to go the extra mile to keep things safe for our patients yet again. We all hope that the government and the unions will come to an agreement soon.
This is also the first round of junior doctors industrial action since the annual August junior doctors change over. This means that there is perhaps more uncertainty around the numbers likely to strike, but I’m pleased to report that our hospitals have yet again done a fantastic job of planning for this.
It’s important to say that we have not seen any increase in incidents or complaints during previous strikes and the absolutely focus of consultants in keeping our emergency and inpatient areas safe, plus the increased space for patients due to lower walk in attendances and less elective activity means that in previous rounds we’ve paradoxically seen a dramatic improvement in emergency access.
So what with this and all the work we’ve been doing on discharge, I’m pleased to report that we have been able to de-escalate from most areas, including going back to having six people in a six person bay at Norfolk and Norwich University Hospitals NHS Foundation Trust. This is really positive news and testament to the hard work of health and care staff across the system.
Compared to our official standard bed base, a few months ago we had around 200 patients in surge or escalation beds – treatment rooms, day rooms, two in a side room, 7 in a six bedded bay, using day case areas and so on. We are now at 70 across all our providers (3 acute hospitals, our mental health trust and both community trusts) so clearly things are going in the right direction.
The bad news though, is that we have had to cancel and rearrange huge numbers of appointments, procedures and operations because of this. These have been stood down to allow the staff who would have been doing them, to cover the work usually done by our junior doctors, during the repeated rounds of industrial action. So while we are mitigating the risk for our emergency and inpatients, I’m much more worried about the risk of harm and poor experience for those patients who have already waited far longer than we’d like. This is a much bigger risk for us as a system now.
We also need to acknowledge the effect this is having on our staff. The moral injury of not being able to provide the care you want to, and also to those admin staff tasked with contacting patients to tell them that their long-awaited admission has been deferred – in some cases for the third time. This is an incredibly difficult position for all of our staff, as well as being very disappointing and worrying for so many of our patients too. And this is happening in all health and care systems across the country.
To put this into context, here’s a summary of the number of people waiting to be seen for planned and elective care at the moment:
- We currently have two patients waiting 104 weeks or more
- 78 weeks – we were almost able to clear these at the end of March but since the industrial action, this has risen again. NNUH has done a real blitz of these this month, which is amazing considering the industrial action going on, but currently have 417 patients waiting over 78 weeks across our three hospitals. We are absolutely determined to clear these very long waits as soon as we possibly can
- 65 weeks: We have 3,646 patients currently waiting over 65 weeks, which is the cohort that we will be focusing on as soon as we have been able to clear the lists of people wiating over 78 weeks, but this continues to be a balance, with emergency, cancer and urgent cases always taking priority due to clinical need.
Primary Care, specifically general practice
Nationally, access recovery planning guidance now been published. Essentially, the NHS as now been given three core priorities; primary care, elective and Urgent and Emergency Care recovery.
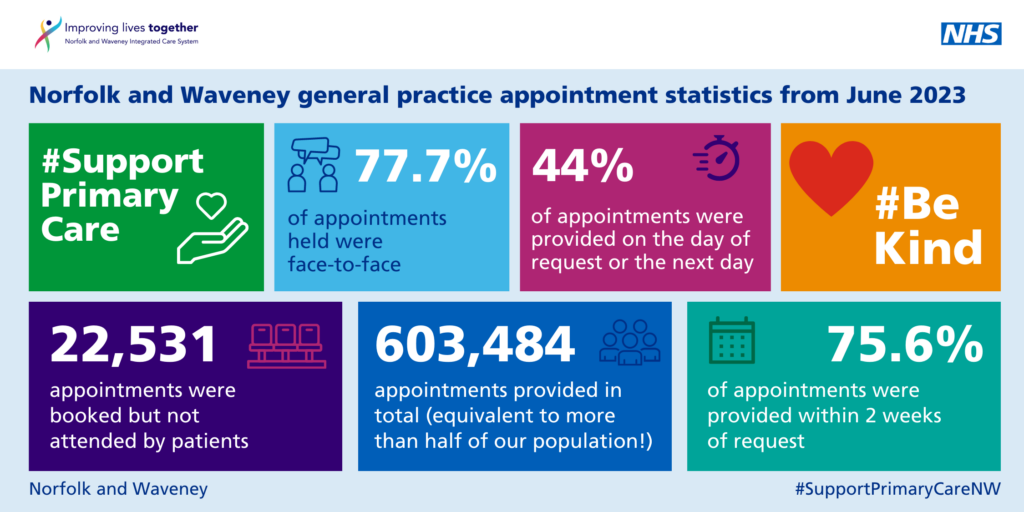
Activity remains extraordinarily high for general practice in Norfolk and Waveney. For June 2023:
- 603,484 total appointments across general practice; equivalent to more than one appointment for every 2 members of our population this month.
- We continue to have slightly lower than same day appointments than nationally at 38.1% same day, but that is almost certainly because we have a much higher proportion which are face to face compared to the national average (77.7% compared to 69%), and a higher proportion of our appointments are with GPs as opposed to other extended roles
- The handy little visual below provides a summary of activity across general practice in Norfolk and Waveney.
The national GP Satisfaction survey was also published last month with some very good feedback for our practices. Despite what you may hear, we have been rated the highest in the East of England for how easy it is to get through to your practice on the telephone; 55% rated this element good or better. And, the overall experience of using our GP practices is joint top, with Suffolk and North East Essex for the East of England at 58% good or better.
On that note, bearing in mind the huge numbers of patients whose appointments are being rescheduled due to industrial action, please do remember that they should never be signposted back to general practice if their hospital appointment has been changed. Patients should always contact their consultant secretary if they are concerned that their clinical condition has changed or worsened since they were last seen at the hospital, or if they have questions about how long they are likely to wait. They should not be told to ask their GP as their GP won’t know how long it will be, and that will only waste a precious appointment.
NHS Norfolk and Waveney ICB restructure
In line with the letter from NHS England in March 2023 unfortunately, we have had to identify ways to save 30% running costs, around £6 million, as well as other work to address about a 30million funding challenge across the whole of our system. So, things remain significantly pressured for us.
So, we will be a smaller organisation and won’t be able to do everything that we previously did. But, we’ve tried to refocus our operating model on the statutory functions of ICBs and the priorities in our recently published, system wide joint forward plan.
A staff consultation was launched on 20 July, so all ICB staff now have the opportunity to feed back on these proposals. We are committed to working with our staff and the wider health and care system to make sure we have got these proposals right. If we haven’t, we will change these to ensure we are resourced accordingly, within our financial envelope, to support and lead elements of transformation, improvement and redesign of our health and care system across Norfolk and Waveney.
In other news
I wanted to put a shout out for our colleagues at James Paget University Hospital NHS Foundation Trust. The latest survey undertaken by the Care Quality Commission last September shows that the JPUH Emergency Department has been given a score of 8.3 out of 10 for overall patient experience, the highest rating in the country. This is an amazing achievement.
Finally, I am delighted to welcome Andy Griffiths to my team, my new deputy. I am sure you will see and hear from him in the weeks and months ahead.
Andy will lead on Clinical and Care Professional leadership engagement, veterans’ health and more. So please give a big warm welcome to Andy when you meet him.
Thank you for everything you continue to do – as always, it is very much appreciated.
Best wishes,
Frankie
