I’d like to begin this month’s blog by wishing a Happy New Year to you all. I hope you all managed to get some time off to rest, recuperate and energise for what’s to come in 2024.
In my first blog of this year, I’d like to provide key updates on:
- Urgent and Emergency Care (UEC), winter and junior doctors industrial action
- Ageing Well
- Clinical and Care Professional (CCP) survey
UEC, winter and junior doctors industrial action
As you will all be aware, we have just finished two recent rounds of industrial action by junior doctors over the Christmas and New Year period.
I would like to thank all colleagues who have worked so hard during this period, and to those who worked differently to help provide safe care for patients who needed urgent and emergency services, as well as those receiving inpatient care in our hospitals. With each round of industrial action, we try to minimise the impact on elective activity and to plan ahead as far as possible but the impact for patients on our waiting lists is still huge and we did unfortunately have to cancel a few appointments on the day, including cancer surgery. These persistent rounds of industrial action are also exhausting for staff and have a huge impact on our people working across our system and on patients awaiting elective work.
My clinic was cancelled this time and so I worked on the wards at the Norfolk and Norwich University Hospital (NNUH) during the latest round. I was really struck by the pace of work on the wards, and the determination to discharge patients safely the moment they were ready to leave. I am so pleased that despite industrial action, this winter has felt very different to what we have previously experienced during what is generally considered to be one of our busiest periods in the NHS.
Not only are all NHS staff working together and working well across primary care, our emergency services as well as our community, mental health and acute hospitals. But the way in which colleagues in the county council, and other across community and social care work with us feels very different this winter – and I think that we feel more like one team than ever. Working together, we have been able to transform complex discharges. There are still too many patients who no longer meet the criteria to reside (C2R) in an acute bed and who are awaiting support to go to the right place. However, this number is down by around 200 compared to this time last year thanks to the work coordinated through our ‘Right Care Now’ board, led by our Executive Director of Nursing, Tricia D’Orsi.
To put into context last week’s figures, we had a total of 434 cases who no longer met the C2R across the three acute providers, and of these, 240 who were on a P1-3 pathway, compared to 640 last winter.
Similarly, last winter, we tended to achieve around 30 complex discharges in a day, but during the IA, we hit a new record with 72 complex discharges in one day in the centre of our patch with 58 of them from the Norfolk and Norwich University Hospital. This is an amazing improvement and I’d like to thank Norfolk and Suffolk County Councils, Norfolk Community Health and Care, East Coast Community Healthcare and other colleagues working across the care sector for helping us to achieve this.
But we’re not stopping there. A new unified digital system, OPTICA, should be live across all three acute trusts from the beginning of February which will help speed up the transfer of care processes even more.
The change in working practice to address ambulance offload delays also continues to make a massive impact. Up until November, we held the largest number of ambulances for the longest number of hours at a single hospital in the whole of England. This has now stopped, and this now means that ambulances are released so that they can respond to emergency calls from our community much more quickly. This is an outstanding achievement and will have saved lives and massively improved the experience of patients and their families right across our community. There is a price to this – we do have more people being cared for in hospital escalation areas and corridors, which is what we are all trying so hard to address with the work on discharge, but the incredible positive impact this has had on reducing ambulance delays cannot be underestimated.
My hopes for this year, will be that consultant members will support the proposals currently put to them by the union, and that the government and BMA can make progress with the juniors and specialist, associate specialist and specialty (SAS) colleagues. We need them back at work to support colleagues and to provide the care we want for all of our patients. But we also need them happier, feeling valued and supported with pay and conditions that will retain them long term.
Winter Infection, Prevention & Control (IPAC) issues
IPAC issues are roughly as expected for this time of year.
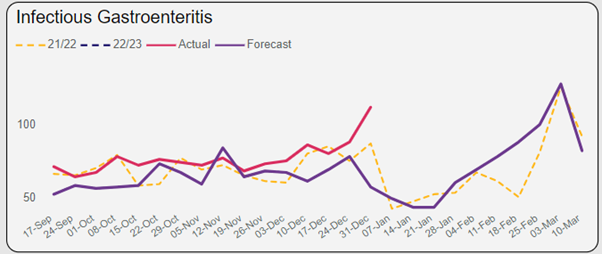
Norovirus and infectious gastroenteritis levels are currently above forecasted levels with a peak in presentations anticipated in early March from modelling based on previous years activity levels.
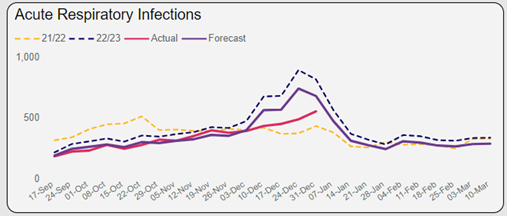
Flu, COVID and acute respiratory infections are at their peak now in terms of Emergency Department (ED) and primary care attendances. But it looks as though the acute respiratory infection hubs we stood up in the community are working well as the number of people attending our EDs is lower than predicted. Bronchiolitis in children peaked early this year and is now roughly as expected. Although bed closures are minimal now, these IPAC concerns meant that a lot of beds were closed during December and added additional pressure within the system.
Impact of winter and IA on Elective recovery
Clearly a lot of elective patients have had their care delayed due to winter and IA related pressures. However, two new paediatric theatres have opened at NNUH this month. These not only offer a fantastic new facility for children to receive care, but also release a lot more capacity in the main theatre complex for other challenged specialties e.g. gynaecology.
The national PIDMAS (patient choice) scheme should also help with our longest waiting patients. While many patients don’t want to travel to have their care provided by another team elsewhere, additional funding has been made available to pay for travel and accommodation costs. This means that some of our longest waiting patients should be having their surgery (e.g. in orthopaedics and gynaecology) provided outside of our region in the coming months.
We are also continuing to explore digital support (e.g. Digital pre op assessments) and sharing best practice to improve our internal productivity. We continue to expand capacity whenever we can e.g. for CT capacity by using the community diagnostic centre in Wisbech, though the biggest challenge for us as ever is staffing particularly in oncology across the system.
As part of the combined acute clinical strategy, in readiness for EPR and the run in to the New Hospital Programme, all of our specialty teams are now working towards becoming clinical networks across our three hospitals. This will mean that we can pool our resources, combine our processes and learn from each other, so that each specialty will work more like one team across different sites.
Ageing well
This has been a novel project for us! We have now held two successful workshops involving a large number of older people with a lot of representation from Voluntary Community and Social Enterprise (VCSE) as well as colleagues from the NHS, public health and social care providers.
We want to bring all providers together to simplify and unify what we provide. But we also want to do things very differently and the feedback provided from our older people was very much that they want to be empowered and listened to in the planning and delivery of care, with a massive shift on prevention.
So, we’ve held workshops, focus groups and a huge number of interviews and this month we held our first formal board at which we recommended our new strategic framework for approval.
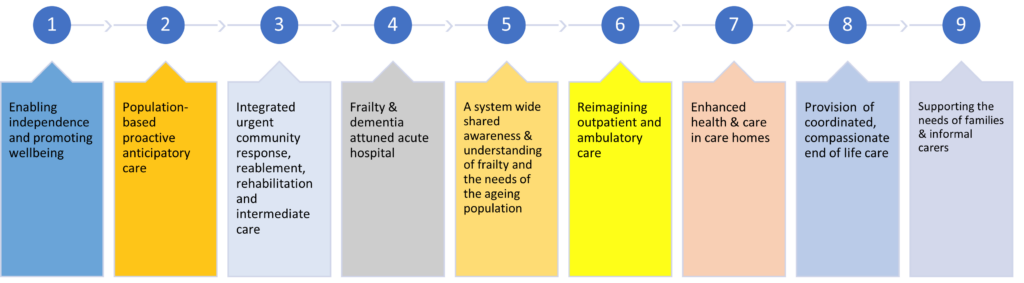
The framework encourages all of our providers and places to focus on how they provide support to people in three phases: prevention and preparing for older age, healthy active older age, and frailty. The more we do together, to support prevention, the more we hope we can extend that healthy active older age and compress the time spent in frailty.
- The framework also outlines 9 areas of work as outlined below, but the priority workstreams for this year will be prevention, dementia, frailty attuned hospital care, and care in care homes. Independence and wellbeing,
- Population based proactive care,
- Integrate urgent community response, reablement and intermediate care,
- Frailty and dementia attuned hospital care,
- Shared understanding of frailty and needs of older population,
- Reimagined outpatient and ambulatory care,
- Enhanced health and care in care homes,
- Coordinated compassionate end of life care,
- Supporting the needs of families and informal carers.
Finally, CCP leadership
The ICB is now 18 months old and so we have been working on this framework for a while now. In line with our manifesto, we have just repeated our annual pulse check to see how CCPs think we are doing and what they want us to do next.
Increasingly, people reported that their organisational CCP leadership mostly/completely reflects the diversity of the community it serves. Also, people felt able to regularly share learning, and 46% feel their current CCPL networks are somewhat /very effective.
However, only 14% feel that the ICB is very or extremely effective at supporting staff to become CCP leaders of the future – so we clearly need to focus our efforts in this area.
A lot of other specific themes also came out from this survey:
1. Communication and Engagement
- Theme: Colleagues emphasise the need for effective communication and engagement strategies including clear and digestible information, along with relevant and targeted engagement.
2. Funding and Time Protection:
- Theme: Consistent mention of the importance of funding, protecting time, and providing adequate resources.
3. Leadership Development:
- Theme: Recognition of the need for leadership development and training at all levels, both formal and practical
4. Role Modelling and Representation:
- Theme: The significance of role modelling and the need for wider representation.
5. Demonstrating Impact and Progress:
- Theme: A call for demonstrating tangible impact and progress resulting from clinician engagement.
6. Visibility and Recognition Efforts:
- Theme: Emphasis on increasing visibility, recognizing contributions, and creating a culture of appreciation.
7. Accessibility and Inclusivity:
- Theme: The need for inclusive engagement methods, accessible forums, and accommodating diverse needs.
8. Feedback Mechanisms and Flexibility:
- Theme: Suggestions for effective feedback mechanisms, flexibility in engagement, and responsiveness to diverse needs.
9. Empowering Clinicians:
- Theme: Calls to empower clinicians through involvement in decision-making, representation on boards, and support for leadership roles.
We are continuing to review this and our work programme to make sure we address as much of it as we can.
Please have a look at here for more details on this, or more information on specific education offers can be found here.
So, to round up, January 2024 feels very different to January 2023. Despite the challenges in particular with the impact of industrial action on all of us, we are working more closely and better than ever before and we can see and feel the positive impact of that. We are also moving our focus more to prevention, in particular in the sphere of ageing, and our CCP programme aims to support our staff, in particular to help them grow as leaders so that they can continue to lead, innovate and improve our services.
I thank you all for your continued dedication and positivity as we strive to maintain the very best integrated services for our patients across our system.
Best wishes,
Frankie
