Well, it’s certainly been another very busy start to the year – and can you believe that it’s the middle of February already! As always, I wanted to start my blog with a recap on our immediate system wide priorities and provide an update on some of those. A huge amount of work continues to address these and, in most areas, we’re making significant progress.
The five immediate system priorities we set ourselves as an ICS for this winter are:
- Mental Health Transformation
- Urgent and Emergency Care (UEC) Transformation
- Elective Recovery and Improvement
- Primary Care Resilience and Transformation
- Improving Productivity and Efficiency
As many of you will know, we are now working on a Joint Forward Plan. Looking at initial feedback so far from our staff, people and communities, as well as looking ahead into how we can help people lead longer, healthier and happier lives, two additional priorities have been added; these are Prevention, Population Health Management (PHM) and Inequalities and Children, Young People and Maternity.
This month, I’ll focus on primary care and UEC, and I think it would also be useful to touch on some developments around PHM, virtual wards, older people and our system wide, Clinical and Care Professionals Programme.
Primary Care
The latest data published shows that for December 2022, the overall trend of demand on primary care continues to rise.
However, compared with national figures we continue to do exceptionally well in the following areas:
- The percentage of face-to-face appointments continues to slowly rise, latest data shows a total of 74.7% of total appointments, compared with 74.2% in November 2022. This compares to a national average of 68.3% appointments being face-to-face
- We also continue to deal with massive urgent and emergency demand in primary care. With the proportion of same day appointments also continuing to rise at 42.9% of all appointments in December 2022, compared with 36.4% in November 2022
- The total number of patients seen in primary care in December was over 560,000 – to put this into context, this is the equivalent of at least one for every two members of our entire population across Norfolk and Waveney. That’s 14% more patients seen than in the same month in 2019 to give a feel for the scale of these increases. To add, the total number of appointments has been a higher number, every consecutive month for the last year except for July where the numbers were basically the same compared with 2019.
- And none of these figures include our world class vaccination programmes!
Primary care support
Last month, I summarised various schemes we have in place or are planning to support primary care, from additional funding, changes to commissioning arrangements, expansion of community services, and the pastoral support available, so I won’t go through this in detail again this month. But, I’d also like to share some welcome signs from our Health Education England and workforce data.
Despite a long term trend that shows the number of GP partners is falling, in Norfolk and Waveney, we are seeing an increase in the number of salaried GPs, as well as an expansion in a number of other primary care roles. And, there has also been a rise in the number of GPs in training since 2018. While this poses difficulties in terms of training provision and supervision during their training, the first people to reach CCT from that increase are now starting to join our workforce. The curricula of our newer medical schools are also very focused on supporting general practise, so whatever is happening nationally, I think we do have some reasons to be optimistic here in Norfolk and Waveney.
Urgent and Emergency Care:
Key themes
- The number of positive COVID-19 in-patients in our hospitals is still falling slowly. At the time of writing (Tuesday 14 February 2022), this figure currently stands at 101 across all providers and Flu has very much waned now, with a total of just 9 in-patients with Flu across all providers now. Whilst these numbers are significantly lower, it is important that staff continue to access flu vaccinations particularly
- Escalation and surge beds, as well as corridor care continues to be used flexibly. 164 additional beds were in use as of Tuesday 14 February
- The total figure for patients without a criteria to reside across our health and care system is 499, though this varies daily
- Three separate tranches of funding have nationally been made available to support patient discharge and system flow since September 2022.
- Demand and capacity fund – £11m (£9m revenue £2m capital)
- Better care funding – £11m combining ICB and NCC allocation
- £3.7m Discharge fund.
Together this has led to the implementation of just over 500 beds (or bed equivalents) across health and social care this winter. While this has been helpful, the community capacity and wrap around care needed to help support, monitor and then discharge these patients’ home has also been stretched.
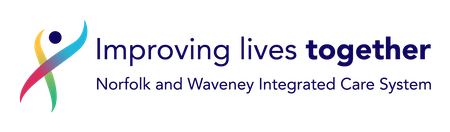
- In addition, we continue to have escalation beds open at all of our main providers, but we are definitely seeing a fall in the long length of stay numbers, and the work to improve our discharge processes has had a real impact. HSJ analysis of discharge delays demonstrates that we are one of the most improved systems nationally in this area.
- We have definitely seen flow and ambulance offload delays improve, and together this has allowed us to deescalate from our critical incident as the highest risk, of very prolonged waiting times for ambulances has improved.
- We are determined to get out of those escalation areas, in a planned fashion, as soon as it is safe to do so. This is likely to happen when we are confident that we can maintain flow, as well as having a very minimal impact on our much improved ambulance response times.
The chart below shows a summary of changes in the number of patients with delayed discharge since latest national funding announced – this analysis was completed by the HSJ of all ICSs, published on 13 February 2022. We are currently sitting third most improved in the country.
As a system, we continue to coordinate all of our UEC work through a dedicated UEC programme board. As a reminder, we have five workstreams ongoing:
- Discharge
- Same day emergency care and in hospital processes
- Urgent community response around preventing the need for admission
- Urgent treatment centres and GP streaming again to reduce demand on EDs
- Virtual Wards
As you know, we have Virtual Wards in place at all of our acute hospitals, but we are also gearing up for massive expansion and transformation of these in particular with ‘step up’ care being launched from April 2023 to complement the existing ‘step down’ care. This is a really great example of system working as we have procured a single home monitoring solution for all of our teams to use. Our providers are working together to provide a really joined up team and service from April 2023.
Elective recovery
We continue to work incredibly hard on this – like UEC pressures, we need to tackle demand as well as capacity.
So, on the demand side we are optimising referral pathways advice and guidance, continually reviewing and risk assessing those waiting and by providing care in the community rather than at acute sites wherever we can.
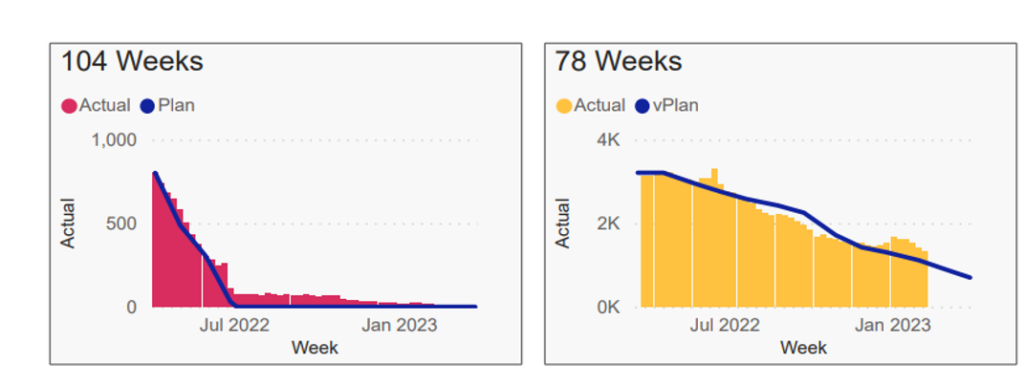
Capacity wise, we are focusing on GIRFT recommendations, in particular the HVLC programmes, and are doing all we can to eliminate all waits of over 78 weeks by April 2023. This is incredibly hard, as of course we need to balance this delivery with UEC demand, the impact of industrial action, and the need to clinically prioritise urgent and cancer cases, but working together, I’m optimistic that we will achieve this aim.
We are also taking every opportunity to bid for funding, for extra diagnostic capacity, not just for imaging, but for blood tests, ECG, spirometry, foot checks, extra operating theatres, elective wards and much more.
The total waiting list size for patients waiting over 78 and 104 weeks for Norfolk and Waveney as of 6 February 2023 can be seen in the two charts below. So, this has been a massive challenge, but we are generally on track with the targets set.
Population Health Management and Public Health
As part of our commitment to prevention, reducing inequalities and improving the health of our entire population, I am very pleased to announce that two members of the Norfolk County Council public health team, Suzanne Meredith and Dr Abhijit Bagade have now joined the NHS Norfolk and Waveney team.
Suzanne will be leading our Population Health Management work for NHS Norfolk and Waveney and supporting the entire system as the lead on development and implementation of a new PHM strategy.
Integrated care of older people
I am also delighted to report that we are setting up a system wide programme board to look at how we can better integrate the care for older people in our system, focusing on prevention and easy access to early intervention. I have reached out to multiple different stakeholders this month and hope to launch this new board in March 2023.
Clinical and Care Professional leadership – exciting new roles available
In line with our manifesto, we are determined to empower and support our CCPs to drive innovation and improvement across our system.
We have just completed a review of all of our decision-making structures to make sure that we build in the voice of CCPs into each of them and our CCP Assembly launched last month to provide a sounding board and consultative forum for our ICS.
We have also taken stock of all the areas where we would like dedicated CCP leadership in and the advertisement for these Specialty Advisor roles is out now.
These new roles are based around our key priorities: primary care, elective recovery, mental health, UEC, population health management and CYP, as well as strengthening the CCP leadership for each place and for each strand of the CORE20PLUS5 agenda. They will also support a number of additional key areas unique to our population based on public health data such as end of life and care of older people.
Please do have a look at the CCP landing page which carries our manifesto, rolling leadership programme and lots more details of how to get involved.
Workforce Support and Industrial Action
These are really difficult times for all of us, and more strike dates are likely to be announced again soon.
Please take a look on the dedicated section of the ICS website is available including the latest information, along with a dedicated frequently asked questions section. This provides the most up to date source of information for our system.
And please use our #WeCareTogether website as your single point of access for free health and well-being resources, free for all staff.
As always, thank you for everything you continue to do.
With best wishes,
Frankie