Clinical Strategy – Year 1 – “You said, we did”
Background
The Clinical Strategy for Norfolk and Waveney is based on the experiences, hopes and ideas of the patients who use the NHS, the staff that work in it, and the communities that it serves.
The strategy represents an important voice, but it is one of a number of equally important voices that include finance, quality, digital health, estates and the wider integration agenda.
It was developed with a wide range of patients, citizens, clinical and care professionals and supported by Healthwatch Norfolk, to signal what our population and our staff told us we want the NHS in Norfolk and Waveney to focus on over the next five years.
It was published in July 2022 after extensive engagement and the six statements that you can see here describe what our plan will try to achieve.
In Norfolk and Waveney My NHS will:
- See me as a whole person,
- Be one high quality, resilient service,
- Reduce long waiting times,
- Act early to improve health,
- Be reliable,
- Tackle health inequalities.
Year 1 achievements
We undertook a huge array of work in year one, with 34 actions, many of which have now been completed or built into business as usual for our teams. In summary,
- 15 are complete.
- 7 are now “business as usual” for our teams so will not be monitored specifically through the clinical strategy from now on although they are ongoing.
- 2 are being managed elsewhere or are part of long-term projects but are not directly relevant to specific clinical priorities within the strategy.
- 10 actions from year 1 are carried over into year 2 because they are still live and are being extended and developed, and we have cross checked where there is overlap with the Joint Forward Plan (JFP) so we do not duplicate.
We published a progress report against Year 1 of the Clinical Strategy in July 2023, which can be found here.
Here are some examples of last year’s completed actions:
- See me as a whole person
You said: I only want to have to tell my story once
We did: We have introduced the Shared Care Record (ShCR) across Norfolk and Waveney. This means that doctors, nurses, social workers and other health and care staff working across our system have access to a shared electronic care record saving time for our staff and meaning that people don’t have to keep telling their story over and over again. This includes GP practices, Norfolk County Council, our community trust, mental health trust and our three acute hospitals.
Further information on ShCR can be found here

2. Be one high quality resilient service
You said: We want organisations to learn from success and challenges and improve services, patient safety and treatment options
We did: We have developed and published a Quality Strategy for how we work across the ICS which includes a Quality Improvement workstream. Examples of Quality Improvement activities from this year include a project to reduce unnecessary disposable glove use across all health and care settings. This reduces infection, saves money and improves our environmental impact. Another Quality Improvement project was with care homes to encourage residents to keep hydrated, aiming to improve quality of life, reduce falls and prevent some urine infections. Quality Improvement work is shared at a bimonthly meeting of all system partners and the NHS East of England regional team to make sure that learning is shared.
Further information on our Quality Strategy can be found here
3. Reducing long waiting times
You said: It is important that patients who are on a waiting list are actively cared for
We did: We have introduced initiatives to ensure that patients waiting a long time for routine operations such as hip or knee replacements are contacted regularly, and that they are reviewed to make sure that they have the support they need to “wait well”. For example, with home adaptations, weight loss and physical activity advice or support to stop smoking. We have also brought in a policy so that all patients on waiting lists are assessed regularly in case their clinical condition and risk has changed since they were added to the waiting list, which would mean that their appointment should be brought forward. We have developed many resources for patients to help them understand waiting lists, to prepare for hospital consultations and treatments, and to support them to wait well with the While You Wait website. We have also provided information on waiting times for specific procedures on the national My Planned Care site.
Further information on waiting well can be found here
Information on waiting times for procedures can be found here

4. Act early to improve health
You said: We should focus on reducing health inequalities across N&W
We did: Working closely with Public Health colleagues in Norfolk and Suffolk County Councils, the Population Heath Management and Health Inequalities Board has been set up to oversee all of the work to act early to improve health and to reduce inequalities. One workstream is focusing on reducing smoking in pregnancy which is known to improve the health of the baby as well as supporting the mum to be and the rest of the family to stop smoking to improve their future health outcomes. All three maternity units at the NNUH, JPUH and QEH King’s Lynn have smoking cessation leads, all maternity staff are receiving specific training and a tobacco dependency treatment service will be in place by April 2024.
Further information on this project is available here
5. Be reliable
You said: We should reduce the number of cancelled appointments.
We did: We have introduced a personalised out-patient (POP) programme across our hospitals. People used to be sent an appointment through the post, sometimes many months in advance. Then, if the clinician wanted to book leave for any reason, or if there were other staffing challenges, the hospital would cancel that and send out another new date, again without checking that it was suitable for the patient. Now, patients are contacted to mutually agree a time and date that is suitable for them for their first appointment and 6 weeks before any follow up appointments are due to reduce the chance of either the patient or the hospital needing to cancel it later. We have also brought in Patient Initiated Follow Up (PIFU) appointments, so patients can request a follow up appointment if and when their condition changes and they feel they need to see their specialist, rather than every patient being invited to come at a set interval.
Further information on PIFU is available here
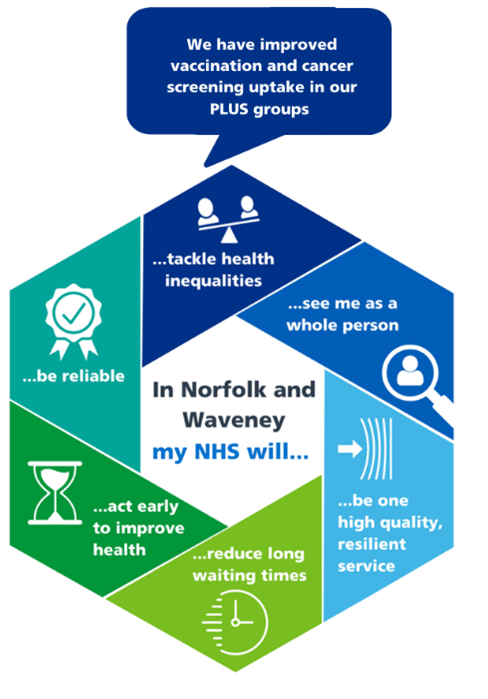
6. Tackle Health Inequalities
You said: Improve screening uptake.
We did: We are undertaking a broad range of work to tackle health inequalities, and to specifically support people in the most deprived 20% of our population as well as a range of PLUS groups. These include the nationally defined inclusion health groups and also specific groups at increased risk of health inequalities in our area such as people living in coastal and rural communities, veterans, members of the armed forces and their families, and people living with learning disabilities or autism.
This year we worked with the Community Voices Partnership to be trusted communicators with local people in these and other groups, to better understand reasons why there is hesitancy in using health services. This has helped us increase uptake of bowel cancer screening, and vaccinations, as well as offering targeted lung checks to people who smoke in Gt Yarmouth and Lowestoft. You can read more about our work to address health inequalities here
Ambitions for Year 2
We have simplified our plans for Year 2, keeping the six statements about what My NHS will do, but each of these has a specific focus this year. Under each focus area we have a series of actions.
Together, these make up 19 new actions for this year, as well as 22 actions relating to these statements which are already included in our Joint Forward Plan (JFP):
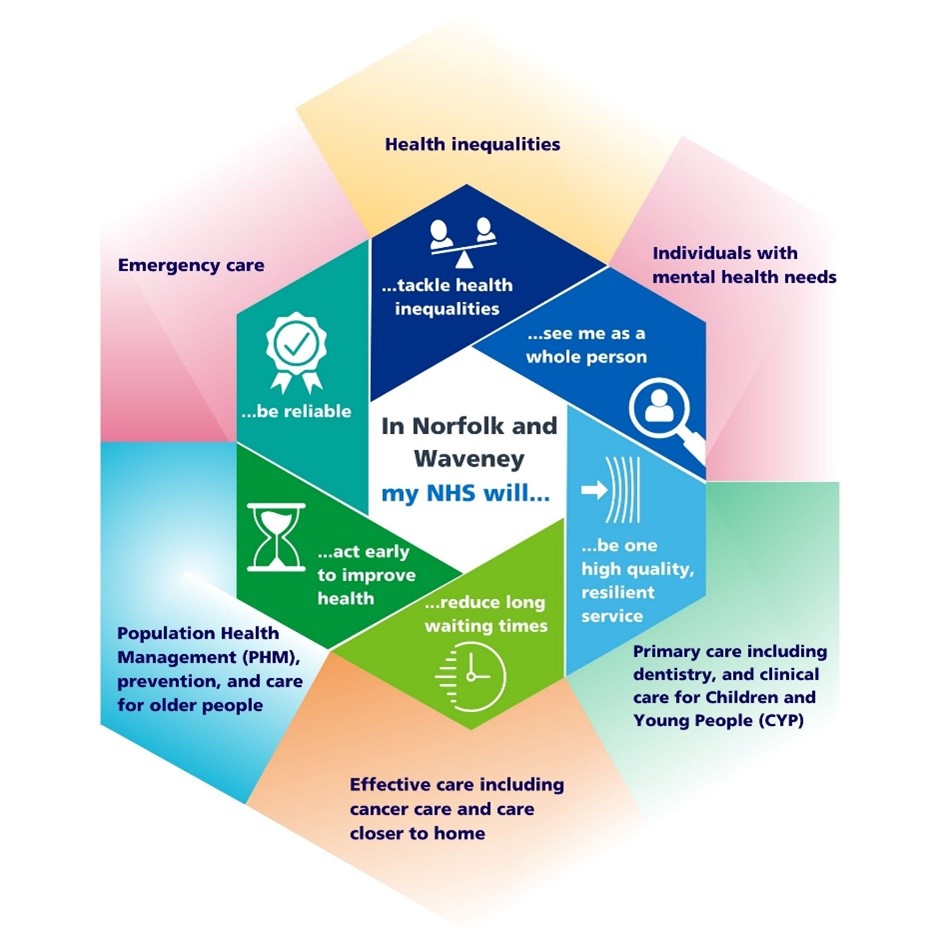
The specific actions for each of the six statements are explained in this section below:
See me as whole person: Focus on people with Mental Health Needs
- Collaboratively review and redesign current Community and Crisis Mental Health Teams
- Focus on the integration of newly developed services into the Crisis and Community pathways
- Commission a Personality Disorder (EUPD) pathway to reduce ED attendances and Community Mental Health Team
- Plus 4 relevant objectives from the JFP. Ambition 4 of the JFP is to transform mental health services
Be one high quality, resilient service: Focus on primary care including dentistry, plus clinical care for Children and Young People
- Support primary care to implement modern general practice access, including use of digital tools, making it easier for patients to contact their GP practice
- Improve access to emergency dental care for children and adults – increased hours and number of surgeries that offer emergency slots daily
- Improve access to prevention and dental care for our local population
- Support people with COVID – long covid clinics, 111 enabled and community provided covid medicine delivery units so there is care closer to home
- Implement shared care record (SCR) roll out to all sectors
- Plus 3 relevant objectives in the JFP around Children and Young People and 2 in relation to general practice and dental service. Ambition 2 in the JFP is about Primary Care Resilience and Transformation and Ambition 3 is to Improve services for Babies, Children and Young People and to develop our Local Maternity & Neonatal System.
Reduce long waiting times: Focus on elective care including cancer care, and care closer to home
- Develop elective surgery centres to help deal with hospital waiting lists.
- We will make a major investment in diagnostic capacity in line with the Richards Report
- Implement personalised outpatients and Patient Initiated Follow Up (PIFU) to all 3 acute trusts, increase proportion of outpatients moved to PIFU
- Dermatology: Redesign and standardise our current dermatology and skin cancer pathways. The case for change will be detailed in a business case, which will be drafted for Q2 2024/25. In the intervening period expand and improve access to dermatology care in the community, e.g. through teledermatology and specialist Advice and Guidance
- Eye Care: Implement a transformation plan to redesign long term eye care conditions with greater integration between community and hospital, and increased use of community care where possible, to enable care closer to home, especially for long-term conditions that require regular follow-up plus reduce demand and waiting times for specialist treatments.
- Plus 2 existing objectives from JFP about elective recovery. Ambition 7 in the JFP is about Elective Recovery and Improvement.
Act early to improve health: Focus on Population Health Management, prevention and care for older people
- Working in partnership across the system on primary prevention to reduce smoking, improve physical activity and support healthy weight management. We will continue to ensure that governance and process becomes well established to progress this agenda, together with ongoing evaluation.
- Decrease falls and improve fracture prevention
- Standardise the assessment for frailty and use of the comprehensive geriatric assessment across Norfolk & Waveney hospitals
- Plus 7 existing objectives from the JFP. Ambition 1 in the JFP is about Population Health Management, Reducing Inequalities and supporting Prevention and Ambition 5 is about Transforming Care in Later Life.
Be reliable: Focus on emergency care
- Improve how quickly ambulances arrive for emergencies in our community: Achieve a category 2 30-minute mean response time by the end of March 2024.
- Improve the flow through our hospitals so that people are admitted and treated more quickly: Achieve or exceed the national target to reduce hospital occupancy to 92% or less.
- Expansion of virtual ward beds so that people can avoid hospital admission completely, or have as much of the care previously delivered in hospitals, provided at home instead.
(These 3 objectives are also in the JFP as part of Ambition 6 – Improving Urgent & Emergency Care)
Tackle Health Inequalities
- Increase Covid, influenza and Pneumonia vaccination rates for those with respiratory conditions such as Chronic obstructive pulmonary disease (COPD) or other clinical risk factors within inclusion health group communities using a variety of different innovative approaches.
- Increase Bowel cancer screening uptake for inclusion health groups through programmes such as the Innovation for Health Care Inequalities programme for Bowel Cancer screening within underserved communities utilising community voices and connectors and outreach approaches.
- Improve the rates of cervical and breast screening uptake for Inclusion Health groups utilising the Inclusion Health locally commissioned service (LCS) specification working collaboratively with Primary Care.
- Plus JFP objective of the publication of a system wide Health Inequalities Strategy to deliver the CORE20Plus5 approach by the end of March 2024. This is part of Ambition 1 in the JFP – Population Health Management, Reducing Inequalities and Supporting Prevention.
Next Steps
We will report progress against these actions internally every 3 months and publish updates every 6 months. Our clinical strategy was first published in July but to make reporting easier in future, we will now align reporting against this strategy to the financial year (April to March), as this is how we report on our other work including the Joint Forward Plan.
We may add new actions during 2024/25 as we close these ones, but we aim to retain these six areas of focus against each of the six ambition statements from here on, as they align well with our wider objectives and our 5 year Joint Forward Plan.
